I. TREATMENT OF INFECTIOUS DISEASES
1. Smallpox and After: An Early History of the Treatment and Prevention of Infections
The scientific work that led to the discovery of the causes of infections was possibly the major biomedical advance of the nineteenth century. From it was derived the aseptic technique of Lister, the use of antitoxins and immunisation, and the ultimately successful search for chemicals selectively toxic to bacterial cells.
The conquest of most of the infectious diseases is, however, the field subjected to the most derisive attack by the antivivisectionists. The scourges that were responsible for the high childhood mortality up to the end of the nineteenth century were, it is claimed, defeated by improvements in sanitation, nutrition and housing, rather than knowledge obtained from animal experimentation.
Improvements in public health undoubtedly contributed to the reduction in death from infectious disease. Obviously the easiest way to avoid morbidity is to stay away from the cause. However, with one notable exception, the causes are still with us. The tubercle bacillus, streptococcus, poliovirus etc. could still, even in our sanitary environment, cause lethal or crippling conditions if there was no appropriate medical intervention. The fact that 50 million prescriptions for antibiotics are written per year in the UK is testimony to the continued prevalence of infective disease.
Pasteur and others, in the second half of the nineteenth century, attributed the cause of certain diseases to microbes that enter (or infect) the body. Pasteur’s subsequent work, on the examination of the relative virulence of microbes after in vitro culture, put a sound scientific basis beneath the empirical practice of smallpox vaccination that was current in Europe at the time.
Smallpox
Those who may harbour in their imagination an affinity for the romanticism of pre-Victorian times would find the historical descriptions of smallpox sobering reading. De la Condamine (1) wrote in 1754:
Every tenth death was due to smallpox, and one fourth of mankind were either killed by it, or crippled or disfigured for life. The disease was a river that everyone had to cross.
This severe scourge was endemic in China and other eastern countries centuries before Christ and was certainly present in Europe in the sixth century.
Bishop Gregory of Tours was surely describing smallpox when he wrote in 582 of the epidemic with vesicular eruption (lues cum vesicis) which began with sickness, fever and back pains. The fever abated with the copious eruption of hard, white vesicles which were very painful. Bad cases were fatal (amongst the young especially) on the 12th to 14th day.
The prevalence of the disease in these early times is indicated by the first clear description of smallpox by a physician. This was that of Isaacus Judaeus, or Isaac the Jew, who lived in the ninth century. Isaac theorised, since smallpox attacked everyone, that it was a natural fermentation of the blood in children in order to get rid of an impurity acquired in the womb. That smallpox continued to be a widespread scourge up to the time of the formal record of morbidity and mortality is evidenced by the quotation of De la Condamine (see above).
Against this background it is not hard to understand the development of the technique of inoculation (or variolation). This was the deliberate infection of pustular matter, collected during a mild epidemic, into an incision in a healthy child. This practice stemmed from the clinical observation that one attack of smallpox conferred protection against the disease and was long used by physicians of ancient China and India. It was introduced into Europe in 1721 by Lady Mary Wortley Montague, wife of the British Ambassador to Turkey. Although efficacious, the procedure was extremely dangerous, causing at least three epidemics on the continent and being fatal in at least 1-2% of cases (2). That individuals were prepared to accept discomfort and such severe risks attests to the inevitability with which people accepted smallpox in the era before any statistics were available.
Jenner’s experiments, published in 1798, obviated the need for variolation and set the scene for the eventual eradication of smallpox. The story is familiar. Jenner, like others before, was intrigued by the accepted belief that individuals who came into contact with the comparatively rare disease of cowpox were immune to smallpox. In his classic experiment Jenner inoculated a boy with pus from a cowpox lesion on the hand of an infected dairymaid. Two months later the boy was inoculated with pus from a smallpox vesicle but did not develop the disease. “Vaccination” with cowpox resulted in immunity to smallpox. Vaccination gradually spread throughout Europe during the next hundred years.
The Vaccine
Initially vaccination was usually effected by the use of “humanised” lymph that is a lymph from the pustules of those previously vaccinated. The occasional accidental transmission of syphilis and the lack of sufficient vaccine material to combat an epidemic led to the use of animals to prepare the vaccine. Horses, mules, goats and rabbits were all used at one time to generate the virus. However calves became the standard method to prepare the vaccine, due to the facility with which the supply could be multiplied at relatively short notice to deal with even the most serious epidemic. The potency of the prepared virus was tested by the rapidity with which it could produce lesions in rabbits (3), it was usually also tested on mice to ensure the absence of tetanus bacilli (3).
The Effects of Vaccination
Where the introduction of vaccination was extended the immediate result was “a striking and rapid fall of smallpox mortality” (2). Fortunately the recording of local or national morbidity and mortality statistics became common at this time and thus the beneficial effect of vaccination was immediately apparent.
Sweden was one of the earliest countries to vaccinate extensively. Vaccination began in Lund in 1801 and 25,000 were so treated by 1805. From 1805 on about 20,000 vaccinations per year were performed. Vaccination was made compulsory in 1816. The effect was dramatic. Average annual deaths per million population during the decades 1792-1801, 1802-11 and 1812-21 were 1,914, 623 and 133 respectively (Fig. 1.1).

Fig. 1.1 Smallpox deaths in Sweden, 1774-1900.
Bavaria, in 1807, was the first country to make vaccination compulsory. Smallpox deaths were reduced and the disease became more prevalent in older persons rather than children. This pointed to the necessity for revaccination, which was made compulsory in 1872, after which smallpox virtually died out in that country.
The Netherlands adopted compulsory vaccination in 1873 and an attenuation in smallpox mortality was immediately apparent.
In England vaccination was made obligatory in infancy in 1853 and compulsory under punishment in 1867, although it is alleged that poor technique resulted in unsatisfactory protection. John Simon in 1857 observed that in England and Wales there was “not only an appreciable amount of utterly incompetent vaccination but a very considerable proportion of second-rate vaccination” (6). During the epidemic of 1871 vaccination was enforced by inspectors.
This was followed by a wane in smallpox deaths (Fig. 1.2).
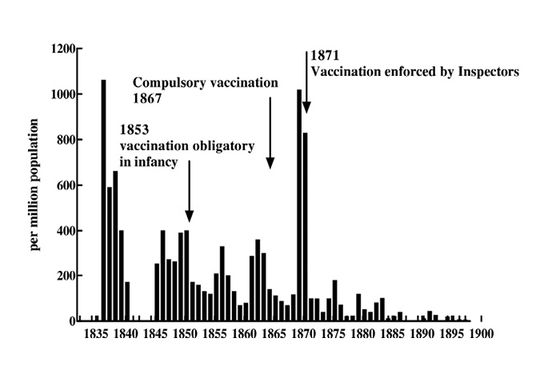
Fig. 1.2 Smallpox deaths in England, 1838-1900 (1843-1846: no reliable data available).
Austria and Belgium had no formal vaccination policy until the last decade of the 19th century and the high mortality from smallpox reflects this.
Most informed opinion would agree with the statement of Zinsser in 1931 (3) that:
The benefits of vaccination are no longer a question of opinion, and opposition to the practice is explicable only on the basis of ignorance.
However others consider that the decline in smallpox occurred throughout Europe despite vaccination (see Ref. 4 for example). One noted opponent of animal experimentation uses carefully chosen figures of death rate from smallpox (although the actual figures are excluded from the graph) to imply that smallpox mortality was declining in England and Wales from 1840-1900 except when vaccination laws were enforced, when there was a dramatic rise (5).
Two factors have enabled those that decry the value of vaccination to muster some spurious evidence to support their claims. Firstly it was wrongly believed that inoculation with cowpox virus would provide life-long protection against smallpox (the protection lasts about ten years). Secondly was the epidemic nature of smallpox, and the fact that a devastating pandemic occurred in Europe between 1870 and 1875. The epidemic began in France and lasted about two years in each country. The occurrence of a sudden epidemic at a time when widespread vaccination was underway is eagerly seized upon as an irrefutable demonstration that vaccination was redundant. However mortality statistics for the years 1870-75 provide clear evidence for the benefits of vaccination, since mortality rates in the countries with vaccination were demonstrably less than where vaccination was not practised at that time. In England the epidemic peaked in 1871 with a death rate of 1,012 per million, in Sweden (where vaccination was started in 1801) 936 per million died in 1874. In Belgium and the Netherlands, where vaccination was not practised the rates were a striking 4,168 and 4,355 per million respectively at the height of the epidemic.
Further proof of the efficacy of vaccination (and of the necessity for revaccination) emerges from the examination of the age distribution of those dying from smallpox (data from Ref. 6). Before vaccination in England, 80% of smallpox deaths were in the younger age groups (under 10 years). As the vaccination of babies spread the ratio reversed, that is those in the older age groups formed the highest proportion of those contracting and dying of smallpox (these individuals had outgrown the immunity conferred by vaccination and of course had not acquired the long-lasting immunity secondary to a mild smallpox infection).
Were it required, additional evidence of the protection by vaccination is provided by the comparison of mortality to smallpox in adjacent countries, one of which had enforced vaccination whilst the other had not (e.g. Belgium and the Netherlands, and Austria and Bavaria).
In the first half of the twentieth century Europe and North America gradually became smallpox free due to extensive vaccination and containment measures (7). Occasional relaxation of vaccination laws always led to outbreaks which had to be suppressed by vigorous vaccination programmes. Zinsser (3) cites an outbreak in Kansas City in 1921 which led to 1,090 cases and 222 deaths. 200,000 people were vaccinated before the epidemic ceased. In 1922 in Denver there was a virulent outbreak of 805 cases with a death rate of over 30%. No order requiring vaccination was issued until November 21, 1922. The result was that there were only 81 cases in December as against 252 in November of that year.
The success of vaccination in eliminating smallpox from countries where it had been endemic raised the possibility of the global eradication of smallpox. This was proposed at the Eleventh World Health Assembly in 1958. After 8 years it was evident that technical and material assistance from the WHO would be required and this was initiated in 1967. Freeze-dried vaccine that met the WHO standards was used and a simplified vaccine technique was devised (the bifurcated needle) that made the programme easier to carry out.
Eradication programmes began in 1967, the last of the remaining 30 endemic countries to start the programme was Ethiopia in 1971 (7).
South America
In 1967 smallpox was being reported almost solely in Brazil. Over 4 years 83.3 million people were vaccinated (90% of the population). Surveillance was begun in July 1969 (which accounts for the apparent increase in incidence at that time) and in 1970 a steady decline occurred until April 1971 when the last case reported.
Africa
At the institution of the vaccination programme (1967) smallpox was endemic throughout South Saharan Africa. By 1972 smallpox incidence had decreased virtually to zero except in Sudan and Ethiopia. After 1971 vaccination and surveillance was increased in these two countries with consequent decrease in cases.
Asia (Mainland)
China had become smallpox free after extensive vaccination in the 1950s and, at the time of the eradication programme, Burma and Iran had only limited outbreaks imported from Asian countries with endemic disease – Afghanistan, India, Nepal and Pakistan.
In these endemic areas surveillance and vaccination resulted in attenuation of the disease which was somewhat slower than in other areas, due partly to the geography and partly to the persistence of variolation, which continued to be practised by itinerant shamans, particularly in Afghanistan and Pakistan.
Indonesia
The programme in Indonesia was started in July 1968 in Java and Bali and was later extended to the remaining islands. By the end of 1971 there were only a few cases in limited foci in Java and one focus in Sulawesi (see Fig. 1.3).
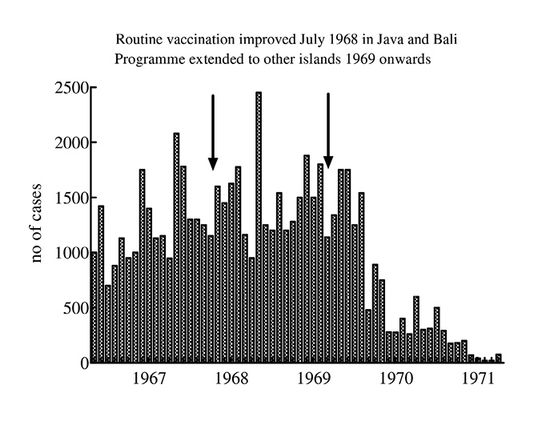
Fig. 1.3 Smallpox incidence in Indonesia, 1966-1971.
Eradication
The last recorded case of smallpox was reported in Somalia in 1977 (8). In view of the long history of the disease this was an astonishing achievement which throws into sharp relief the criticisms of those who claim that vaccination was ineffective (4) and dangerous. The diminution of the disease over a hundred years in both developed and Third World countries immediately after the institution of a vaccination programme either attests to the value of the procedure or is a remarkable coincidence.
As to the dangers of vaccination, the statement by Sharpe (5) – that “vaccination was stopped in 1940 when the considerable risks were thought to outweigh the benefits” – is typical hyperbole. Serious complications of vaccination, according to the WHO (7), were so infrequent that “very large populations must be studied in order to assess the relative risks involved.” In one extensive study in the USA in 1968 (7) there were 9 deaths in over 14 million vaccinations. Five of these occurred either in eczematous patients (eczema was considered a contraindication in non-endemic areas) or in patients with immunological defects.
The Scientific Origins of Immunisation
Whilst the acceptance of vaccination was spreading across Europe, Pasteur and his colleagues were carrying out experiments that were to give rise to the techniques for providing active artificial immunity to many diseases. It is of significance, and somewhat ironic, that the crucial experiments were those carried out into the cause and treatment of diseases of animals – chicken cholera and anthrax.
Chicken cholera
Chicken cholera was a lethal disease that occurred in epidemics in poultry yards. Due to the emerging prominence of the “germ theory” at that time it was thus naturally thought that the cause was a microbe. Pasteur found and described the microbe as: “tiny bodies, extremely slender and constricted in the middle, which would at first sight be taken for isolated dots.”
Pasteur (Fig. 1.4) succeeded in cultivating the microbe outside the body in a neutral, sterilized broth made of ground up chicken meat. Small amounts of the broth sprinkled on the food given to chickens caused the disease, and Pasteur proceeded to demonstrate that the microbe flourished in the gut of the infected chickens, and passed on the infection through the faeces. The microbe was fatal to rabbits on inoculation but when injected into the skin of guinea pigs produced a local abscess. Such infected (but apparently generally healthy) guinea pigs however could spread the disease to both rabbits and poultry (as Pasteur remarked – how many obscurities in the history of contagions will one day be cleared up by even simpler experiments).

Fig. 1.4 Louis Pasteur (1822-1895), microbiologist. Wellcome Library, London, CC BY.
The crucial discovery made by Pasteur was that cultures of the chicken cholera microbes, left for some time, lost their ability to transmit the disease to hens. This was a chance observation due to cultures being left over a vacation. It was typical of the thoroughness of Pasteur that he decided to see if the “ineffective” cultures had produced any change in the condition of the chickens. On administration of a fresh culture these hens proved resistant to the disease. The same operation on hens obtained fresh from the market caused death in them all from cholera.
It was known that recurrence of a virulent disease after survival of a severe attack was rare. Resistance was conferred by the challenge. Pasteur had found a way of producing the resistance without the risk of the disease.
Anthrax
Although the development of a “vaccine” against chicken cholera was of enormous scientific significance the disease itself was not of great importance. Because of long experience of the disease poultry farmers kept birds in small groups and killed sick hens immediately, before the disease could spread. Anthrax on the other hand was a disease of sheep and cattle that was of enormous importance. Each year 5% of cattle and 10% of sheep died of anthrax in France. In some particular areas of France and the Argentine the mortality to farm animals was so great the land had to be left unused.
Using the culture techniques with which he had become expert Pasteur addressed the problem of the prevention of anthrax.
Small bodies, termed bacteridia, had sometimes been detected in the blood of animals suffering from anthrax, but the weight of scientific opinion considered the disease to be due to something invisible termed “virus” (as was the case for smallpox). Pasteur found that the bacteridium would grow freely in neutralised urine. By successive subculture he produced a culture diluted from the original virulent one by many million times. That this culture could still produce anthrax in guinea pigs proved that the bacteridium was the cause, since all else had been diluted out.
By a series of elegant but simple experiments Pasteur showed that the anthrax bacteridium infected sheep through the alimentary canal and also explained how the disease persisted in particular “accursed fields” (champs maudits) where cattle or sheep were bound to contract anthrax if they were allowed to graze.
Koch had shown that anthrax bacteridia could form spores in conditions of high oxygen levels and temperature. Pasteur demonstrated the presence of anthrax spores in the fine top soil of the accursed fields. The spores were brought to the surface (sometimes from the buried bodies of anthrax sheep or cattle) by earthworms. Presumably the animals ingested the anthrax spores from soil contamination of the grass or clover upon which they grazed. Extracts of the soil produced anthrax in guinea pigs even if the soil had been heated to 90oC (which kills off other soil bacteria). Pasteur also produced anthrax in guinea pigs by inoculation of the soil from the intestine of earthworms.
An Anthrax Vaccine
In order to develop an attenuated strain of bacteridia (similar to the innocuous but immunogenic culture of chicken cholera) Pasteur investigated the vitality and virulence of cultures treated in various ways. The bacteridium grew only between 16 and 44oC. When cultured at fairly high temperatures (42-43oC) a very virulent strain grew rapidly but Pasteur found that the virulence waned, so that the culture became harmless to guinea pigs after 12 days, but would kill mice. After 4 weeks even mice and baby guinea pigs survived challenge with the culture.
Pasteur was thus able to produce “vaccines” of graded strength depending upon the duration of the high temperature incubation, and he used these to protect animals against a challenge with a virulent anthrax culture. The stage was set for a field trial.
Pasteur proved the effectiveness of his vaccine with a convincing public demonstration at Pouilly-le-Fort in 1881. Under the supervision of a vet 25 sheep were inoculated with Pasteur’s vaccine, 25 were not so treated. On May 31st all 50 sheep were inoculated with a virulent culture of anthrax bacteridia. The trial was a spectacular success. On June 2nd all the vaccinated sheep were in good health. Of the non-vaccinated, 22 were dead and three dying. The experiment was repeated in 10 cows with the same definitive result.
Of course criticism persisted, particularly from some veterinarians who were offended at the intrusion of a scientist in what they considered their preserve. But when the vaccine was shown also to protect animals against inoculation with blood from an animal dying from anthrax, and “not a mixture of unknown nature made up in a laboratory, and whose constitution no one knows but the makers” – all opposition disappeared.
In France, between 1882 and 1893 nearly 4 million animals received anthrax vaccine, and loss of cattle and sheep from the disease fell to low levels. The use of Pasteur’s vaccine spread throughout Europe and the World. By 1914 40 million doses had been sent out from the Pasteur Institute alone.
By a simple animal experiment, of a style and to an extent that could never be reproduced in humans, Pasteur had shown indisputably that immunisation did protect against infective disease. This protection induced against an animal disease should be held as irrefutable evidence for the value of immunisation – which, of course, is repudiated by the animal rights organisations. It is also evidence that animals themselves benefit from such research. It may be alleged by opponents of animal research that protection against anthrax merely solved an economic problem for milk distributors and wool merchants. However, it undoubtedly prevented animal suffering and such a claim of vested interest cannot be levelled at the research that resulted in a vaccine that conferred protection against canine distemper.
An earlier version of this chapter was published as: Smallpox and after – an early history of the treatment and prevention of infections. RDS News July 1993 5-10.
References
- De la Condamine (1759) Mémoire sur l’inoculation de la petite vérole. Histoire et Mémoires de l’Académie Royaledes Sciences (read at the public session of April 24, 1754).
- Edwardes EJ (1902) A Concise History of Small-Pox and Vaccination in Europe. HK London: Lewis.
- Zinsser H (1931) Textbook of Bacteriology, 6th edition. New York: Appleton.
- Chaitow L (1987) Vaccination and Immunisation: Dangers, Delusions and Alternatives. Saffron Walden: Daniel.
- Sharpe R (1988) The Cruel Deception: The Use of Animals in Medical Research.London: Thorsons.
- Hardy A (1983) Smallpox in London: factors in the decline of the disease in the nineteenth century. Medical History 27 111-38. http://dx.doi.org/10.1017/s0025727300042599
- (1972) WHO Expert Committee on Smallpox Eradication. 2nd Report. World Health Organization Technical Report Series No. 493 Geneva: WHO.
- Paton WDM (1993) Man and Mouse. 2nd edition, p. 77. Oxford: Oxford University Press.
Other sources
Descour L (1922) Pasteur and his Work. London: T Fisher Unwin.
Paget S (1914) Pasteur and After Pasteur. London: Black.
Duclaux E (1920) Pasteur: The History of a Mind. Philadelphia: Saunders.







