16. Packaging Technology
© 2022 Frank Stadler, CC BY-NC 4.0 https://doi.org/10.11647/OBP.0300.16
This chapter is concerned with the packaging of medicinal maggots for sale and transport. After fly eggs have been disinfected, incubated, and the microbial safety of eggs and maggots has been confirmed, medicinal maggots are counted and transferred to primary packaging for safe transit to the point of care. This primary packaging may then be further packaged within a cardboard box that forms the secondary packaging along with package inserts that specify vital product and use information. In addition, when medicinal maggots are transported over greater distances or under unfavourable climatic conditions, insulated transport packaging is essential.
Introduction
This chapter is concerned with the packaging of medicinal maggots post-production and in preparation for transport to the wound care provider. After the eggs are disinfected and incubated, and after the microbial safety of eggs and maggots has been confirmed, medicinal maggots are counted into treatment units—usually in multiples of 50 maggots per unit (e.g. 100, 250, 500). For safe transit to the point of care, they need to be placed into a suitable container that holds a single medicinal maggot unit. Because this container is in direct contact with the product, it is called the primary packaging. In the case of ordinary pharmaceuticals (e.g. tablets) the primary packaging is then further packaged, for example inside a cardboard box, which is referred to as the secondary packaging [1]. For medicinal maggots that are produced at the point of care, for example at a hospital, such secondary packaging may not be necessary, provided that the primary packaging is labelled with all the information that would ordinarily be on both the primary and secondary packaging. However, if a producer supplies medicinal maggots on a commercial basis to customers, then appropriate secondary packaging is desirable to convey essential product information, and to protect the product. In addition, transport of medicinal maggots to care providers that are not located in the same institution where the maggots are produced requires insulated cool-chain packaging. Distribution logistics is covered in Chapter 17 of this book [2].
This chapter follows guidance on the essential requirements for primary and secondary packaging as well as temperature-controlled transport packaging for medicinal maggots. The chapter provides only an overview of the aspects that must be considered when packaging maggots. It is critical that producers confirm with their own national regulators the specific local requirements for the packaging and labelling of therapeutic goods.
Primary and Secondary Packaging
The primary packaging must provide adequate humidity, ventilation and a secure enclosure so that the small, young maggots cannot escape. In addition, the primary packaging must be sterile at the time of packaging and protect medicinal maggots from microbial contamination for the duration of transport until they are applied to the wound. The primary packaging may hold maggots that are either i) provided for free-range application, which means that they are directly placed into the container—with or without a moistened gauze pad, or ii) they are sealed first in a teabag-like net pouch and then placed into the primary packaging [3].
Producers may package medicinal maggots in sterile, hard-shelled pathology sample jars made of plastic, or various other types of laboratory-grade plastic containers of similar volume (Figure 16.1). There is no hard and fast rule, so long as the above-mentioned conditions are provided. The larger the volume of the jar the less need there is for ventilation and tightly sealed containers can be used for primary packaging purposes—but only if there is fast delivery of the maggots at cool temperatures, which slows down maggot metabolism and oxygen consumption. Medicinal maggots die if not adequately ventilated. In addition, larger volume containers result in parcel space being wasted with thin air. Therefore, smaller-volume, slender tissue culture vials or tubes that are fitted with a filter lid, and thereby allow gas exchange, may be used to reduce the volume of packaging, and consequently healthcare waste (Figure 16.1). The primary packaging system may then be packed either directly into a transport box or further placed inside branded secondary packaging that does not inhibit ventilation of the primary packaging.
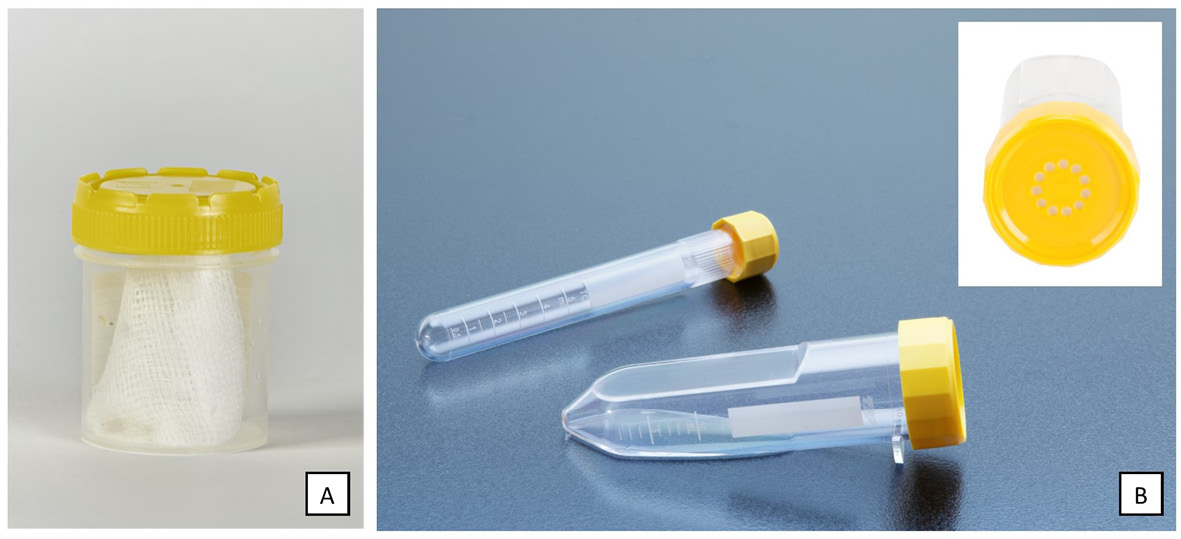
Figure 16.1 Primary packaging containers that may be used for the transport of medicinal maggots: A) Sterile 70 mL pathology specimen jar suitable only for rapid delivery at cool temperatures, unless modified to permit air exchange, B) Tissue culture tubes fitted with a filter lid that permits air exchange while maintaining sterility. Photos by (A) F. Stadler, MedMagLabs and Creating Hope in Conflict: A Humanitarian Grand Challenge, CC BY-ND and (B) © TPP, www.tpp.ch).
Consumer safety is a major concern in healthcare and therefore providers of therapeutic goods need to ensure that their goods cannot be tampered with prior to reaching the patient. In the case of medicinal maggot packaging, this may be achieved with
- a tape seal, a heat shrink band, or a perforated wrapper applied to the primary packaging that will need to be broken in the process of opening the container [4]; and/or
- a tape seal on the secondary packaging box which also reveals any access to the packaging content when broken [4].
Air-tight plastic wrapping around the secondary packaging box must be avoided because it would restrict airflow and ventilation of the primary packaging container and its living content.
As alluded to earlier, the primary or secondary packaging (if used) for medicinal maggots will need to be labelled according to best practice. The World Health Organization (WHO) guidelines on packaging for pharmaceutical products [1] say that the labels on primary/secondary packaging should at least provide the following information:
- the name of the drug product;
- a list of the active ingredients and their amounts;
- a statement of the net contents (number of dosage units, mass or volume)
- the batch number assigned by the manufacturer;
- the expiry date in an uncoded form;
- any special storage conditions or handling precautions that may be necessary;
- the directions for use, and any warnings and precautions that may be necessary;
- the name and address of the manufacturer or the company or person responsible for placing the product on the market.
Ideally, wound care practitioners should be familiar with maggot therapy prior to ordering and receiving medicinal maggots from the producer. A package insert should nevertheless be forwarded with each medicinal maggot consignment or inserted into the secondary packaging boxes. Information provided on the package insert should complement information printed on labels. It must explain to the healthcare practitioner what medicinal maggots are, how to use them, what the indications and contraindications for maggot therapy are, and what potential side-effects to look out for. With the rise in mobile telephony especially in low- and middle-income countries, the package label and package insert may also refer to a website or mobile device application that provide i) helpful treatment information, ii) answer frequently asked questions, and iii) contact details for a helpline in case practitioners require additional guidance.
Counterfeiting. Counterfeit medicines are a growing problem, particularly in developing countries [5]. They imitate the original product and apart from being an intellectual property infringement, counterfeit medicines may be of poorer quality and potency. Because flies are relatively easy to produce, maggot therapy will be vulnerable to counterfeiting in low- and middle-income countries.
The food and pharmaceutical industries seek to prevent counterfeiting with radio frequency identification and one- and two-dimensional barcode technologies, which in turn allow track-and-trace monitoring of batches throughout the supply chain [6]. The Guidelines for Bar Coding in the Pharmaceutical Supply Chain [7, 8] set out best-practice barcode use in the pharmaceutical supply chain. In addition to authentication of products, such bar coding can facilitate the back-tracing of production batches in case of an adverse event during treatment. For example, the Australian Red Cross Blood Service is a bio-medical product supply chain that successfully uses bar code identification and tracking of blood products from collection to transfusion [9]. However, radio frequency identification and other tracking technologies come at an extra cost, which must be borne by the supply chain and, ultimately, the customer [10].
In Nigeria, mobile phone solutions are available for patients to detect counterfeit drugs. A short code found on the packaging is sent via text message to the service provider who then verifies authenticity of the medicine [11]. In addition, the packaging technology itself can assist with the identification of authentic medication. Solutions include packaging design features, security labels, coding, printing and graphics, holograms and forensic markers [12].
Irrespective of these measures, poor patients receiving care from unqualified healthcare providers will be the most likely targets for counterfeit medicinal maggots. Heavy discounting of maggot therapy through a means-tested payment schedule or other financial support from governments and NGOs may be more effective than the above-mentioned counterfeit prevention measures because if the poor are given access to affordable, high-quality maggot therapy products and services, there is little incentive for them to use risky, illegal alternatives.
Having discussed the dangers of counterfeit medicinal maggots and options to guard against fraudulent supply, it must be mentioned that there are situations when such informal entrepreneurial activity might be welcome. For example, modern warfare and conflict increasingly target and affect civilian communities which are consequently impacted by violence, isolation and lack of resources. In such cases, it would be beneficial for isolated, conflict-affected communities to rear their own medicinal maggots to care for casualties and those patients with chronic wounds [13].
Transport Packaging
Temperature Control
Medicinal maggots are temperature-sensitive products. For example, Lucilia sericata maggots will die at temperatures over 47℃ [14], which are easily reached during the summer in vehicles that are not equipped with appropriate air conditioning. At the other extreme, prolonged exposure to cold temperatures below 6℃ can also harm medicinal maggots. Under no circumstance must they be cooled below 0℃ as freezing will kill these fragile organisms. However, cool temperatures at and above 6℃ can be exploited to slow down the maggots’ metabolism in order to arrest their development and extend the period they can be kept without food. Some producers have stored L. sericata maggots at temperatures as low as 4℃ for up to 5 days [15, 16] without unsustainable mortality, but it is now generally accepted that medicinal maggots in transit should be maintained at temperatures between 6℃ and 25℃ and that they should be administered within 24 to 48 hours from dispatch [17, 18].
As Figure 16.2 illustrates, the acceptable temperature range for medicinal maggots in transit and short-term storage ahead of maggot therapy appears to overlap with that of many heat- and freeze-sensitive vaccines, which must be stored at all times between 2℃ and 8℃ [19], and red blood cell products which must be stored between 1℃ and 10℃ [20]. Thus, the management of vaccine and blood supply chains faces the same challenges as medicinal maggot distribution, and this provides opportunities for supply chain collaboration and integration, as well as mutual learning [21].
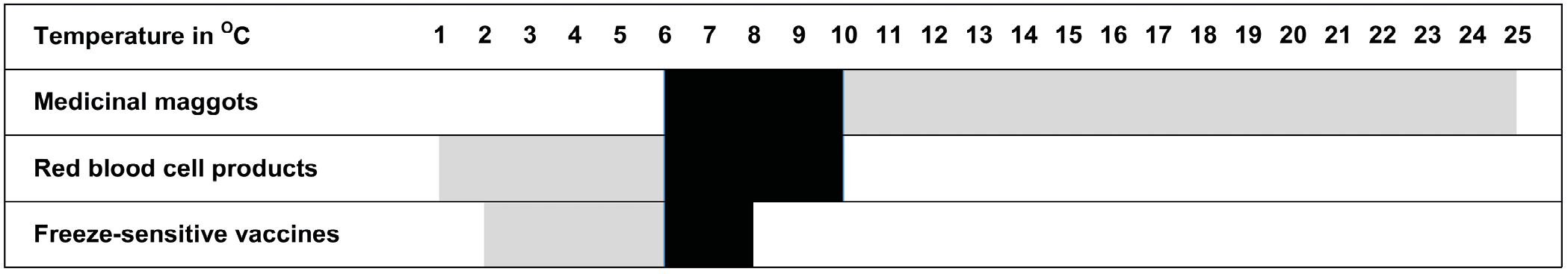
Figure 16.2 Safe temperature ranges for heat-sensitive medical products, including medicinal maggots. The safe temperature range that medicinal maggots share with the other two products is shown in solid shading.
Ineffective cooling with temperatures rising beyond recommended levels has been observed for blood product shipping containers [20, 22]. In the vaccine cold chain, however, it is the accidental freezing of vaccines that leads to frequent and significant vaccine wastage. It appears that vaccine cold chains fail because healthcare workers are insufficiently trained, cold storage and transport equipment is inadequate, and there is an unreliable power supply or other disruptions to refrigeration equipment [23]. In compromised healthcare settings these conditions may be the result of socio-economic disadvantage or armed conflict [24], but they are also encountered in high-income healthcare settings. It is a common observation that there are significant awareness and training gaps in health workers and cold chain system inadequacies in high-, low-, and middle-income countries, and that these put vaccine potency at risk [25, 26]. Consequently, improved training and education, implementation of equipment upgrades, and improved systems and standards can lead to significant improvements in cold-chain management [27–29]. It follows that the performance of medicinal maggot cool chains will also benefit from such measures, especially in compromised healthcare settings.
Cool- and Cold-Chain Packaging Solutions
Heat sensitive pharmaceuticals, chemicals and biologics are generally shipped using disposable cold-chain packaging [30]. These containers are made of highly insulating materials such as polystyrene and cool elements are used to lower the internal temperature to the desired range. Commercial medicinal maggot suppliers in Europe and the United States use such disposable packaging. However, in recent times, multi-use cold-chain packaging solutions have come on the market that are able to maintain the 6–25℃ temperature range necessary for medicinal maggot transport [30]. Moreover, multi-use new vaccine transport container designs also utilise passive cold storage which employs sophisticated insulation, phase-change cooling elements, and precise temperature monitoring [31].
There are economic and environmental considerations when deciding on the best packaging solution for medicinal maggots. Reusable packaging systems have been shown to save money and significantly reduce waste and carbon emissions when compared to disposable packaging [30, 32]. These are important issues to consider when establishing a supply chain, particularly in low- and middle-income countries, because distribution inefficiencies and the need to provide affordable wound care may require more cost-effective distribution solutions. Furthermore, pharmaceutical waste is a significant environmental issue and should be reduced if possible [33–35]. The benefit of reusable packaging in the cold and cool chain has been demonstrated by Eli Lilly who implemented the Credo system of reusable packaging [36] and closed-loop reverse logistics for cold chain shipments using four sizes of shippers. As a result, they reduced the number of shippers per order, achieved a shipper return rate of 96%, reduced waste by 192,505 kg in the first year, and saved $2 million annually [37].
What type of packaging medicinal maggot producers choose will depend ultimately on the transport distance, the environmental conditions encountered in transit and at the point of care, and the number of primary packaging units to be shipped. For example, if a producer only supplies a few local hospitals that are nearby and can be reached by courier or personal delivery within an hour, only very basic packaging is required to keep temperatures at or below 25℃. If the aim is to maintain ideal conditions for 24 to 48 hours because of distribution distance or transport inefficiencies, then more sophisticated cool-chain packaging is required. Packaging systems will also need to be selected to match the volume of shipments. Fortunately, cool-chain packaging comes in a variety of sizes. In practice, wound care providers order one or a few medicinal maggot units at a time, which means that producers require mostly small-volume cool-chain packaging solutions.
Temperature Monitoring and Field Testing of Packaging
Producers are advised to test the performance of their selected packaging before routine use and bulk purchase. This can be done easily and inexpensively with multi-use temperature data loggers [38]. Testing is as simple as sending parcels to customers using the preferred cool-chain packaging that contains i) typical consignments of medicinal maggots, ii) cool elements, and iii) a small electronic data logger that measures and records the internal temperature of the package at intervals. It is important that the data logger is not stored directly next to the cool elements but instead in close proximity to the medicinal maggot primary packaging units. Upon receipt of the consignment, the customer records the date and time of delivery, checks whether the shipped maggots are alive and active at room temperature, and returns the data logger to the producer for analysis. Such testing should be repeated periodically, especially if the producer receives complaints regarding poor-quality maggots or the therapeutic efficacy of supplied medicinal maggots.
Summary
Like most therapeutic products, medicinal maggots will need to be transported from the lab where they are produced to the point of care. If the point of care is located in the same organisation or place, demands on packaging are not so great and simple, sterile primary packaging with WHO-compliant labelling will suffice.
However, for commercial producers shipping medicinal maggots over great distances to their customers, primary packaging that permits ventilation and gas exchange while still protecting medicinal maggots from microbial contamination is required. In addition, high-performing insulated packaging is required to maintain the fragile payload at a temperature range between 6–25℃. Fortunately, there is an ever-increasing array of cool- and cold-chain packaging solutions to choose from. Commercial producers may also like to brand their products with secondary packaging which must not obstruct primary packaging air exchange. Every shipment of medicinal maggots should also be accompanied by a package insert that complements primary packaging labels with vital information about the producer and product such as indications, contraindications, treatment advice, and side-effects.
The establishment of a black market for counterfeit medicinal maggots must be avoided when maggot therapy is introduced to low- and middle-income healthcare systems. Various technologies can be adopted from the pharmaceutical industry, including tamper-proof packaging, radio frequency identification, and phone-based verification systems. Appropriate packaging technology that ensures not only product viability and safety, but also safe use of medicinal maggots once they arrive at the point of care, is a critical part of the maggot therapy supply chain. Importantly, the available packaging technology options determine which distribution systems for medicinal maggots can be established.
References
1. WHO Expert Committee on Specifications for Pharmaceutical Preparations. Annex 9 — Guidelines on Packaging for Pharmaceutical Products. WHO Technical Report Series, No. 902 — Thirty-sixth Report. 2002. https://apps.who.int/iris/bitstream/handle/10665/42424/WHO_TRS_902.pdf;sequence=1.
2. Stadler, F., Distribution Logistics, in A Complete Guide to Maggot Therapy: Clinical Practice, Therapeutic Principles, Production, Distribution, and Ethics, F. Stadler (ed.). 2022, Cambridge: Open Book Publishers, pp. 363–382. https://doi.org/10.11647/OBP.0300.17.
3. Sherman, R., Medicinal Maggot Application and Maggot Therapy Dressing Technology, in A Complete Guide to Maggot Therapy: Clinical Practice, Therapeutic Principles, Production, Distribution, and Ethics, F. Stadler (ed.). 2022, Cambridge: Open Book Publishers, pp. 79–96, https://doi.org/10.11647/OBP.0300.05.
4. TGA. Code of Practice for Tamper-evident Packaging of Therapeutic Goods. Version 2.0, May 2017. https://www.tga.gov.au/sites/default/files/code-practice-tamper-evident-packaging-therapeutic-goods.pdf.
5. Hollein, L., et al., Routine Quality Control of Medicines in Developing Countries: Analytical Challenges, Regulatory Infrastructures and the Prevalence of Counterfeit Medicines in Tanzania. TrAC Trends in Analytical Chemistry 2016. 76: pp. 60–70, https://doi.org/10.1016/j.trac.2015.11.009.
6. Rotunno, R., et al., Impact of Track and Trace Integration on Pharmaceutical Production Systems. International Journal of Engineering Business Management, 2014. 6, 25: pp. 1–11, https://doi.org/10.5772/58934.
7. GS1, GS1 General Specifications. The Foundational GS1 Standard that Defines How Identification Keys, Data Attributes and Barcodes Must Be Used in Business Applications. Release 17.0.1. 2017, GS1. https://gs1it.org/content/public/58/d7/58d73d56-ebc1-4372-b6f0-e5d7d0a5abcc/gs1_general_specifications_v17.pdf.
8. HDMA, HDMA Guidelines for Bar Coding in the Pharmaceutical Supply Chain. 2011.
9. Australian Red Cross Blood Service, The Australian Guidelines for the Labelling of Blood Components Using ISBT 128. 2020, Australian Red Cross Blood Service. https://www.lifeblood.com.au/sites/default/files/resource-library/2021-12/94.-ISBT128-Australian-Guidelines-V9-final-30032020.pdf.
10. Schapranow, M.-P., et al., Costs of Authentic Pharmaceuticals: Research on Qualitative and Quantitative Aspects of Enabling Anti-counterfeiting in RFID-aided Supply Chains. Personal and Ubiquitous Computing, 2012. 16(3): pp. 271–289, https://doi.org/10.1007/s00779-011-0390-4.
11. Taylor, N. Sproxil & Orange Fight for Anti-counterfeiting Market in Kenya. 2011. https://www.outsourcing-pharma.com/Article/2011/10/13/Sproxil-Orange-fight-for-anti-counterfeiting-market-in-Kenya.
12. Zadbuke, N., et al., Recent Trends and Future of Pharmaceutical Packaging Technology. Journal of Pharmacy & Bioallied Sciences, 2013. 5(2): pp. 98–110, https://doi.org/10.4103/0975-7406.111820.
13. MedMagLabs. Creating Hope in Conflict: A Humanitarian Grand Challenge. http://medmaglabs.com/creating-hope-in-conflict/.
14. Richards, C.S., B.W. Price, and M.H. Villet, Thermal Ecophysiology of Seven Carrion-feeding Blowflies in Southern Africa. Entomologia Experimentalis et Applicata, 2009. 131(1): pp. 11–19, https://doi.org/10.1111/j.1570-7458.2009.00824.x.
15. Baer, W.S., The Treatment of Chronic Osteomyelitis with the Maggot (Larva of the Blow Fly). The Journal of Bone and Joint Surgery. American Volume, 1931. 13: pp. 438–475, https://doi.org/10.1007/s11999-010-1416-3.
16. Sherman, R.A. and F.A. Wyle, Low-cost, Low-maintenance Rearing of Maggots in Hospitals, Clinics, and Schools. American Journal of Tropical Medicine and Hygiene, 1996. 54(1): pp. 38–41, https://doi.org/10.4269/ajtmh.1996.54.38.
17. Čičková, H., M. Kozánek, and P. Takáč, Growth and Survival of Blowfly Lucilia sericata Larvae under Simulated Wound Conditions: Implications for Maggot Debridement Therapy. Medical and Veterinary Entomology, 2015. 29(4): pp. 416–424, https://doi.org/10.1111/mve.12135.
18. BioMonde. Application Guide and Daily Care Plan. 2015. http://biomonde.com/attachments/article/7/BM197_EN_03_0115.pdf.
19. Lloyd, J., et al., Reducing the Loss of Vaccines from Accidental Freezing in the Cold Chain: The Experience of Continuous Temperature Monitoring in Tunisia. Vaccine, 2015. 33(7): pp. 902–907, https://doi.org/10.1016/j.vaccine.2014.10.080.
20. Webster, J., I.M. Croteau, and J.P. Acker, Evaluation Of The Canadian Blood Services Red Blood Cell Shipping Container. Canadian Journal of Medical Laboratory Science, 2008. 70(5): pp. 167–176.
21. Stadler, F. Supply Chain Management for Maggot Debridement Therapy in Compromised Healthcare Settings. 2018. Unpublished doctoral dissertation, Griffith University, Queensland, https://doi.org/10.25904/1912/3170.
22. Lippi, G., et al., Suitability of a Transport Box for Blood Sample Shipment over a Long Period. Clinical Biochemistry, 2011. 44(12): pp. 1028–1029, https://doi.org/10.1016/j.clinbiochem.2011.05.028.
23. Samant, Y., et al., Evaluation of the Cold-chain for Oral Polio Vaccine in a Rural District of India. Public Health Reports, 2007. 122(1): pp. 112–121, https://doi.org/10.1177/003335490712200116.
24. Obradovic, Z., et al., The Impact of War on Vaccine Preventable Diseases. Materia Socio-Medica, 2014. 26(6): pp. 382–384, https://doi.org/10.5455/msm.2014.26.382-384.
25. Rogie, B., Y. Berhane, and F. Bisrat, Assessment of Cold Chain Status for Immunization in Central Ethiopia. Ethiopian Medical Journal, 2013. 51 Suppl 1: pp. 21–29.
26. Yakum, M.N., et al., Vaccine Storage and Cold Chain Monitoring in the North West Region of Cameroon: A Cross Sectional Study. BMC Research Notes, 2015. 8, 145: pp. 1–7, https://doi.org/10.1186/s13104-015-1109-9.
27. Fernando, M., An Analysis of Clinical Risks in Vaccine Transportation. British Journal of Community Nursing, 2004. 9(10): pp. 411–415, https://dx.doi.org/10.12968/bjcn.2004.9.10.16111.
28. Mallik, S., et al., Assessing Cold Chain Status in a Metro City of India: An Intervention Study. African Health Sciences, 2011. 11(1): pp. 128–133 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3092313/.
29. Turner, N., A. Laws, and L. Roberts, Assessing the Effectiveness of Cold Chain Management for Childhood Vaccines. Journal of Primary Health Care, 2011. 3(4): pp. 278–282.
30. Forcinio, H., Packaging Addresses Cold-Chain Requirements. Pharmaceutical Technology Europe, 2014. 26(10): p. 54.
31. Chen, S.-I., et al., Passive Cold Devices for Vaccine Supply Chains. Annals of Operations Research, 2015. 230(1): pp. 87–104, https://doi.org/10.1007/s10479-013-1502-5.
32. Hartman, L.R., Pharma Packs Sustain Temperatures and the Environment: Walmart Specialty Pharmacy’s Thermal-management Shippers Maintain Temperatures, Regardless of the Weather, Are Sustainable and Cut Shipping Costs by 50 percent, in Packaging Digest. 2008, UBM Canon LLC. p. 50.
33. Oke, I.A., Management of Immunization Solid Wastes in Kano State, Nigeria. Waste Management, 2008. 28(12): pp. 2512–2521, https://doi.org/10.1016/j.wasman.2007.11.008.
34. Patwary, M.A., W.T. O’Hare, and M.H. Sarker, An Illicit Economy: Scavenging and Recycling of Medical Waste. Journal of Environmental Management, 2011. 92(11): pp. 2900–2906, http://dx.doi.org/10.1016/j.jenvman.2011.06.051.
35. Sartaj, M. and R. Arabgol. Quantitative Assessment and Statistical Analysis of Medical Waste Generation in Developing Countries: A Case Study in Ifahan (Iran). Iranian Journal of Science and Technology-Transactions of Civil Engineering 38: C2, 409–420, 2014. http://ijstc.shirazu.ac.ir/pdf_2418_9216d0a563d024c0edad2e847dd29774.html.
36. Pelican. Credo — Reusable Passive Thermal Packaging. http://www.pelicanbiothermal.com/products/credo.
37. Mohan, A.M. Study: Reusable Pharma Packs ‘Greener’ than Single Use. 2013. https://www.healthcarepackaging.com/article/sustainability/reusability/study-reusable-pharma-packs-greener-single-use.
38. PATH. Temperature Monitoring Devices: An Overview. 2013. http://www.path.org/publications/files/TS_opt_handout_tmd_overview.pdf.