9. Creating and Sustaining the Care Information Utility–How, Where and by Whom?
© 2023 David Ingram, CC BY-NC 4.0 https://doi.org/10.11647/OBP.0384.05
We come now to the most challenging questions concerning the care information utility: how, where and by whom will it be created and sustained, and under what governance arrangements? This chapter looks to the wider and future scene, to consider how the work described in Chapters Eight and Eight and a Half can be extended and sustained, in the context of greater opportunity and need for individual self-management of care and supportive services that move from a fragmenting culture of ‘What is the matter with you?’ to an integrative culture of ‘What matters to you?’ We must embrace an iterative and incremental approach here, where we learn by doing. The chapter is thus not prescriptive; it rather reflects on the nature of the challenges faced and what we should have in mind in framing our policy and practice in tackling them.
Central to this will be the approach and method adopted for implementation of a coherent and trusted information utility that every citizen can feel part of and contribute to, which helps and supports them along the way as they seek health and wellbeing in their own lives, and the lives of those they care for. The chapter highlights the importance of the Creative Commons and public domain governance that bridges with and preserves the non-exclusive relationship with private enterprise. The story of common land and its appropriation to private interests through the eighteenth-century Enclosure Acts in the UK, is visited as a parable of common ground in the Information Age. It discusses the harm that restriction of intellectual property does in blocking innovation that tackles intractable ‘wicked problems’, which require connection and collaboration on common ground, within diversely connected communities of practice.
The chapter then focuses on the work of implementing and sustaining the care information utility and the environments, teams and communities whereby it is enabled and supported. It looks at the different qualities of leadership that such pioneering endeavours require and exemplify, and playfully compares them with the principles outlined in The Art of War, the classic text of Sun Tzu, which is much used in elite management courses on leadership. With its focus on people and environments, this part of the chapter draws a great deal on people I have known and worked with, and environments we worked in and created together, and is thus especially personal and autobiographical.
Trust in and recognition of individual and communal roles and responsibilities must unite citizens with the multiple professions and communities of health care practice, around shared goals for the care information utility. Governance arrangements will thus constitute a third major component of implementation of a utility that is coherent, effective, efficient, equitable, stable and life-enhancing, in support of health care services for the Information Society of tomorrow.
These threefold challenges of implementation will require strong alliances–the theme I reflect on, in parenthesis, at the end of the chapter.
Bolder adventure is needed–the adventure of ideas, and the advantage of practice conforming itself to ideas. The best service that ideas can render is gradually to lift into the mental poles the ideal of another type of perfection which becomes a programme for reform.
–Alfred North Whitehead (1861–1947)1
When spontaneity is at its lowest, in practice negligible, the final trace of its operation is found in alternations backwards and forwards between alternate modes. This is the reason for the predominant importance of wave transmission in physical nature.
–Alfred North Whitehead2
I repeat this first quotation to re-emphasize that care information utility is an adventurous idea and a central focus in the reform and reinvention of health care. It is a shared resource, created, owned, operated and sustained locally. It is not a directed flow from a source to a recipient of information. It is a resource that faces and informs both ways. Governance and rules of the road must reflect this mutuality and be understood, trusted and supported accordingly.
Chapter Eight has addressed questions of what is needed and why. This chapter connects them with the practical question of how. It is about the approach to and method of implementation, and the endeavour and governance that will be required to create, bring to fruition and sustain an evolving care information utility. At the centre of the utility is record, and at the centre of record is the individual citizen. How will this utility be created, based on what approach and method? How will it build on and supplant current fragmented legacy information systems? Why, what and how form a tripod of implementation that frames endeavours–they are about approach and method. They must be learned, not prescribed. I call this tripod Implementation One.
Where, who and when form a further tripod for endeavours. I call it Implementation Two. Where is about environment–the setting in which to tackle the creative and ongoing challenges. Who is about people–teamwork and leadership. When is continuously–the imperative is to keep moving upstream and sustain efforts through staying power. This chapter is thus also, crucially, about the people, teams and wider connected communities needed to co-create, own, operate and sustain the utility, the environments where they collaborate and the common ground they create, occupy and share. These are the good environments that Richard Wollheim (1923–2003) described as not a luxury but a necessity, that are needed for nurturing the utility from sapling tree into forest ecosystem.
Those first two tripods of implementation need a third to balance and stabilize approach, method and endeavour. This is the tripod of head, heart and hand of citizens and communities, expressed through systems of governance. I call it Implementation Three. Good governance, too, must be learned.
In my geometrically and visually configured mind, implementation is thus depicted as a triangle of the three complementary tripods of approach and method, endeavour and governance. It is enacted by people in settings and contexts, imbued by the culture and values they develop and exhibit in their work and behaviour. I have thus cast implementation as a triangle of tripods (implementation, implementation, implementation!) to emphasize its importance–a trifecta of complementary tripods! Making and doing these things, iteratively and incrementally, is all-important. And drawing everything together, at the apex of a tetrahedral implementation pyramid, is indivisible trust. Implementation comes together within a safe and trusted framework of making and doing. Figures 9.1 and 9.2 provide a pictorial representation of this esoteric geometry in my mind!
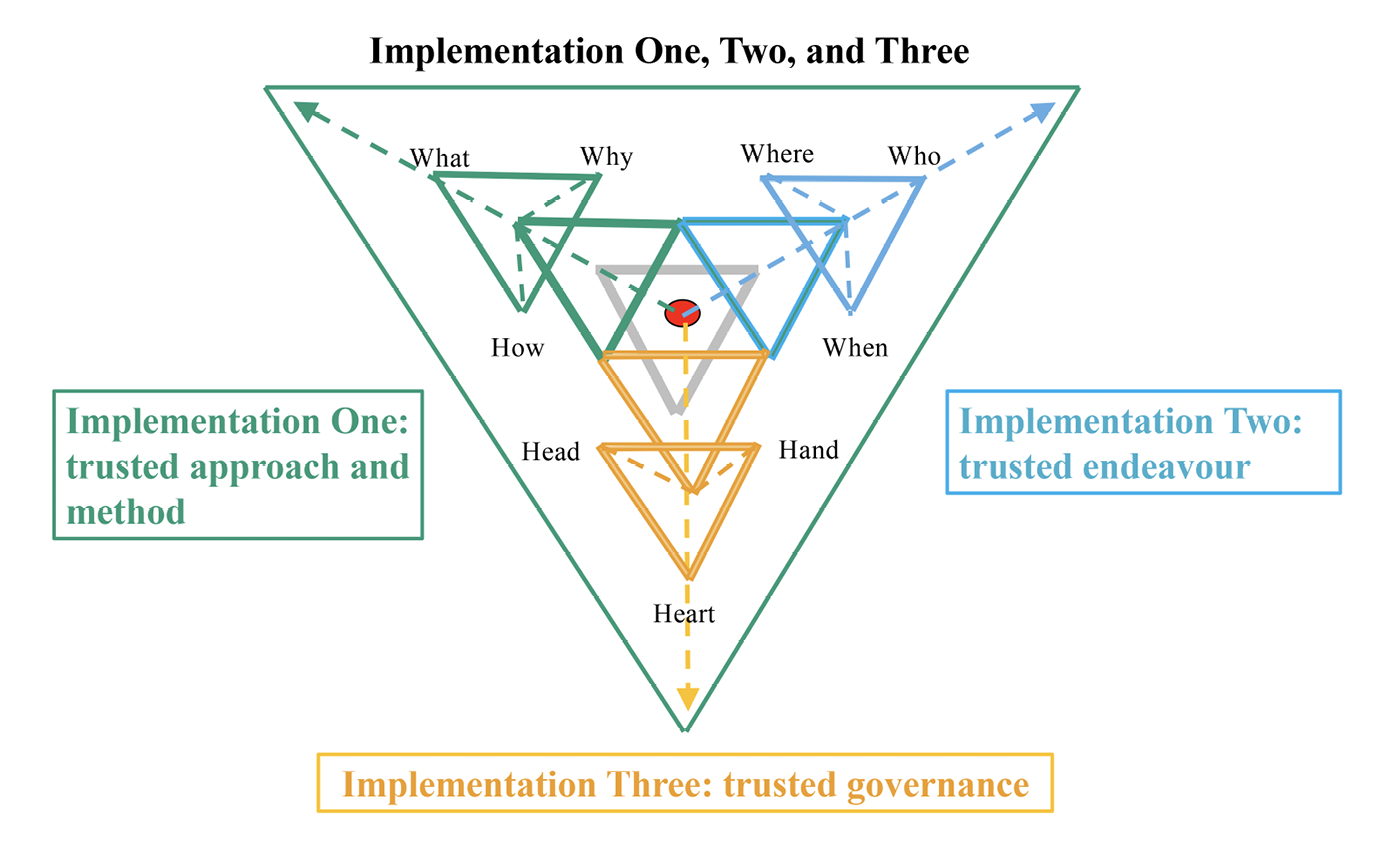
Fig. 9.1 Looking down from the red trust apex of the threefold implementation pyramid. Image created by David Ingram (2022), CC BY-NC.
The Polish mathematician Wacław Sierpiński (1882–1969) was a pioneer of set and number theory and topology. His work has inspired model builders and artists. Images of the fractal decomposition of the Sierpiński tetrahedron have inspired my characterization and illustration of the threefold dimensions of implementation of the care information utility in this chapter.
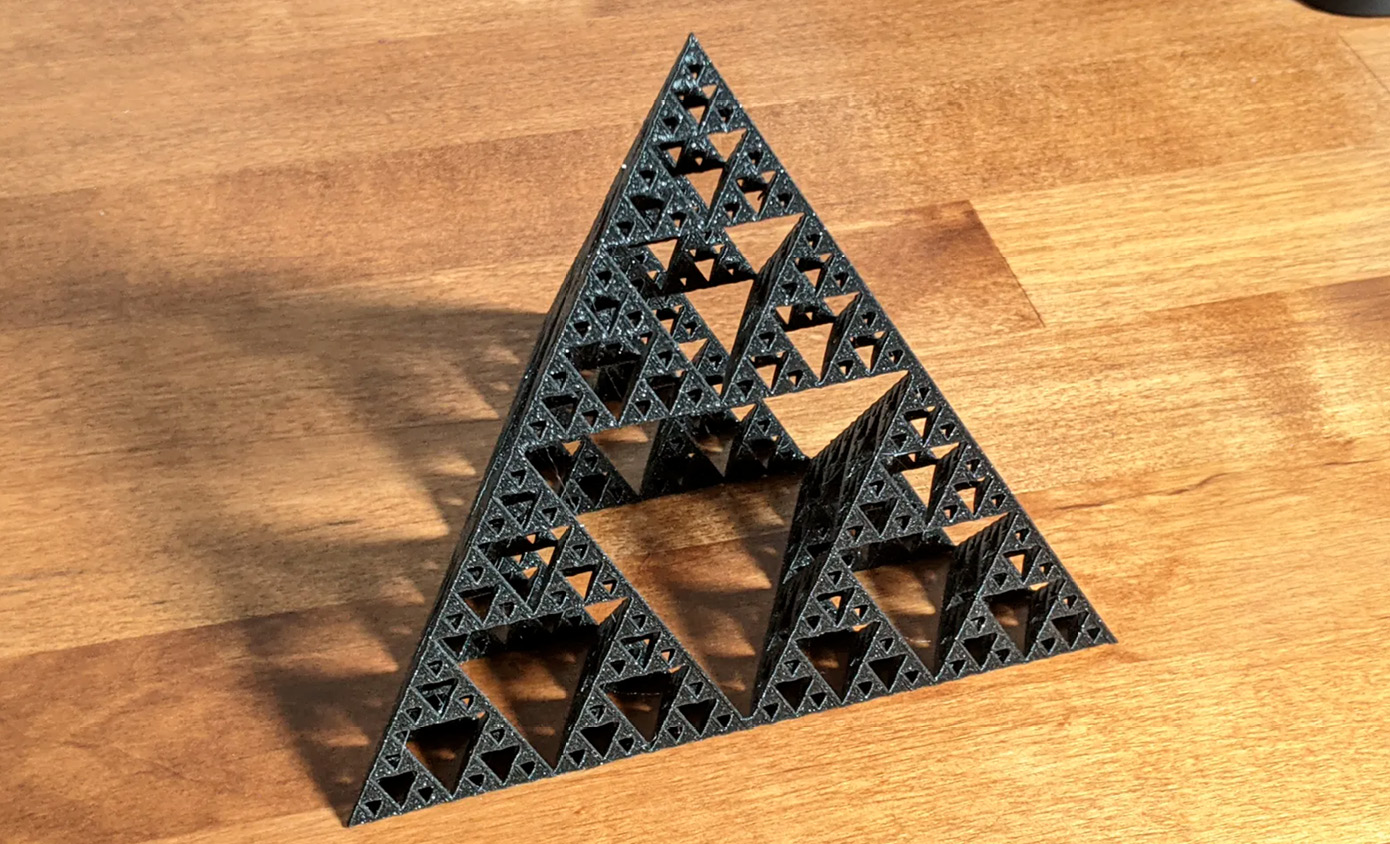
Fig. 9.2 A fractal three-dimensional printed model of the Sierpiński tetrahedron–tetrahedron enfolded within tetrahedron, illustrating the fractal nature of implementations. Based on a design by Josef Prusa (2021), CC BY-NC, https://www.printables.com/en/model/67531-sierpinski-tetrahedron
Enough abstract geometrical analogy! Implementation cannot just be analyzed, planned and managed. It is organic and must be nurtured, grown, led, and sustained, and learned about through example.
We might similarly characterize three dimensions of reinvention and reform of health care services, as matters of approach and method, endeavour and governance. There is continuous interplay along and between these dimensions, that defies prescription and requires resilience to cope with events and adapt as they unfold uncertainly over time. This chapter draws from personal experience of this interplay along my songline, in several different contexts. It compares the ‘horses for courses’ observed and experienced, seeking to highlight patterns relevant for the future. Notwithstanding the pretence of electoral cycles and manifestos, none of this can ever be created with magic bullets or in rapid progress. Controlled nuclear fusion-based power stations have long been fifty years away, and care information utility is a still forming vision and long-term goal!
The quotations from Whitehead that headline this chapter, written a hundred years ago, are still to the point. In the first, he is suggesting that bolder adventure of ideas is needed to guide reform. This complements Mervyn King’s call for new ideas that are approached with audacious pessimism.3 He must have pondered that term–preferable to risk-averse pessimism or audacious optimism, which abound in uncertain times! The second quotation reflects the price we pay when lacking adventure of ideas, common purpose and energy in what we make and do–our actions oscillate to and fro, like waves in a water tank. The politics and policy of health care has oscillated between central and devolved focus, public and private provision and different models of delivery. Expensive reorganizations of associated services have gone through recurrent limit cycles of boom and bust.
King described the recurring crisis of the money and banking systems as a crisis of ideas. In banking, huge sums of money were spent on new information infrastructure and yet the instability of the monetary system persisted and worsened. The lack of ideas that King regretted was not about ways to spend money shoring up infrastructure. It was about lack of ideas for reform of the purposes, principles and goals underpinning the monetary system, as the global economy headed through the Information Age, with the computer exposing and amplifying its vulnerabilities. Care information utility is not about ways to spend money on infrastructure, either. Governments have spent very considerable amounts on computers and consultancy, mistakenly expecting thereby to change and shore up a fragmenting landscape of health care services.4
Some of these fragments have been prioritized and benefited hugely and function much better as a result–general practice IT systems in the UK being one good example. There have also been pre-eminent scientific, technological and clinical advances in imaging systems, genomics and pharmaceutics. Confidence in what artificial intelligence (AI) might contribute is both exploding and imploding, as I write–valiant AlphaFold meets its shifty alter ego, ChatGPT, as it were! Perhaps the Neocene will never be seen, or perhaps it will be us that no longer see. Implementation Three and confident governance resembles St George squaring up to this unpredictable dragon, hopefully equipped with effective armour and a sharp sword!
Leaving such speculative conjecture aside, in terms of what health care information systems could now be, with the individual citizen the central focus, the reality still falls far short of requirement and expectation. Ever more money spent in falling short, makes long-term reform ever harder. Confidence is at a low ebb.
Through the course of the preceding chapters, I have highlighted what I have seen and experienced as historic overemphasis of policy on what is needed and expected from health care information systems, and why, and lack of focus and critical examination of how its vision can be created, governed and sustained. Lacking a practical sense of how desired reform can occur and be sustained, the outcomes sought and invested in are not achieved, and undesired outcomes grow in their place. Implementation of policy has swung like a pendulum, between central fiat and local autonomy; it has been scattered and inconsistent in focus, oblivious to harm done in places struggling to cope and care. It is hard not to feel appalled by and ashamed of the cost, waste and harm it has engendered in many out of sight, out of date and increasingly decrepit environments in which our health care services, and their teams must operate.
Information policy is central to all the professions of health care and those they serve, the ways they work together and are organized, and the information systems and technologies they employ. Approaches to policy focused on prediction and management of goals and targets that have not often been met–as Chapter Seven addressed in detail–and pursued largely devoid of methods for achieving traction, have repeatedly failed to gain traction. This has made successive policy initiatives increasingly hard to implement, being increasingly encumbered and impeded by changing requirements, new science and technology, and a burgeoning legacy of incompatible information models and systems brought into being along the way. This failure has led to poorly contained explosion of noisy information–much as the Octo Barnett-led report to the Office of US Congress Technology Assessment Board feared and foretold, fifty years ago.5
All that said, Richard and Daniel Susskind counselled against what they called ‘technological myopia’, by which they meant the tendency to discount future potential of technology to assist and improve, by emphasizing too greatly its current perceived failings.6 Whitehead described mistakes and failure as normal parts of improvement and growth. All this is true, but simply repeating an ever more expensive and complex failure, revisiting the same ground that has characterized much of the past fifty Groundhog Years, is not acceptable. New ideas are needed, as is deeper and more openly shared reflection on the reasons for successive failures of policy and strategy, and failure to learn from experience, that have characterized policy in the field.
This chapter proposes how we might, and now can, bypass and progressively clean up the costly and accumulating legacy of unconnected and incompatible information systems, to create a care information utility that is much more cost-effective and better positioned along a sustainable pathway for the future, more in tune with the changing times, as we evolve into the Information Society. It proposes an effective, affordable and agile way to approach, create, replenish and sustain this utility, drawing on thirty years of personal experience and effort along the runway. This may, no doubt, be seen by some as a silly, unworldly and naively optimistic vision, perhaps also fearing that it is a destabilizing and threatening one. It has certainly been treated in those ways, but it is still alive and developing, as Chapter Eight and a Half has shown, after those many years of growing pains. I have taken heart from King and Erwin Schrödinger (1887–1961) in expressing it here. New ideas are needed, and we should not shrink from appearing or being cast as foolish in expressing our ideas, especially when we have real-life examples of these ideas being implemented and working coherently in practice and at scale, with connectivity and continuity that has eluded much, and far more expensively unsustainable, practice to date.
Implementation experiences of the architectural blueprints outlined in Chapter Eight and a Half are well advanced along new runways all over the world. And through dint of hard-won and multiprofessional team culture, practical industrial and organizational skill and effort, and staying power, these are amassing achievements that are helping shift the balance to a more open and inclusive way of thinking and acting. If these small efforts, many of the early ones substantially voluntary and unfunded, continue to bear fruit, they will have been very worthwhile. They have been, and probably will still be countered by giga-amounts of money and influence spent on powerful politically and commercially coordinated and focused efforts, with deep pockets and a mix of ambitions for enclosure and control of services and markets. At worst, if they ultimately fail, our now worldwide teams and community will have reset the dial for other communities to think differently and generate their own new ideas, that build and improve on what has been made and done to date. This will be useful learning to have documented, alongside that of the Broad System of Ordering and GALEN Project of Chapter Two. Great movements do fail–the Chartist movement, for example, with its story of community empowerment before universal suffrage. Samuel Smiles (1812–1904), my Chapter Five guide to the transforming power of innovation, as exemplified in the Industrial Revolution, was one of its champions. But, in failing, that movement also moved the dial.
In the parenthesis of Chapter Four, the topic reflected on was purpose. In Chapter Five, it was making and doing things differently. There is little point in having a purpose, unless pursued with commitment, and little point in setting a goal, unless accompanied by a realistic sense of how to achieve it. How, in practical terms, will the care information utility be created? How, likewise, will it work and be maintained and sustained? Implementation is about setting achievable goals and building the communities and environments needed for achieving them. It is about values and principles guiding the approach taken and method adopted, whereby success can be nurtured, and approach and method adapted, in context and over time, to remain focused on the purposes served.
Wicked problems of policy are real and the complexities and difficulties they present must be coped with, as much as predicted and managed. This coping centres on honest communication and competent listening, responsive to needs and recognizing limitations, and creating and building on common ground. It is very much a domain in need of what Gillian Tett, the anthropologist and financial journalist, described in her 2021 book, Anthro-Vision.7 She argues for a different AI–anthropology intelligence not artificial intelligence. She describes new attention being drawn globally to corporate governance focused around ESG (Environment, Social and Governance) principles of sustainability. This is seen as a modern-day imperative, when coping with the VUCA era (Volatility, Uncertainty, Complexity, Ambiguity) which has intensified through the Information Age.
This chapter suggests an audacious idea of care information utility, built on a tripod of co-created and shared intellectual property, community interest and enterprise, and an inclusive balance of global, national and local governance, drawn from these communities. As ever, in a spirit of ‘audacious pessimism’, this must prove its credentials, iteratively and incrementally, and be seen to be realistic, in actions and outcomes, not words. It must prove an agile and flexible approach, adaptable to changing context and need, as science, engineering, health and care, all experience, live through, learn from and emerge from the transition of the Information Age. It must accommodate new balances: of human head, hand and heart, with technology; of professional and personal roles and autonomy; of public and private enterprise; of global and local society and culture.
This is an open and inclusive perspective that seeks to help repair and reunite the prevailing fragmentation of sectors and professions of health care services, and of the organizations, communities and individuals they serve, and those that support them. The policy for several health economies well known to me–usually smaller ones, each serving no more than several million citizens–is aligning and further fostering creation of care information utility along this pathway. As I write, highly innovative tenders for openEHR-based community-wide health care information ecosystems have just been adjudicated for Catalunya, attracting considerable interest among policy makers in other places. Also as I write, a similar tender is being publicized by the Östergötland region of Sweden, potentially spreading more widely across the four or five principal health regions of the country.
I draw on several and disparate sources, in making the case for creating common ground and pursuing openness and collaboration in these endeavours. These reflect social, economic and political circumstances, and thinking that is not new. Such concerns have arisen in much the same way, both in history and in present-day deliberations about other major policy challenges. The first comes from the history of common land and its enclosure in early nineteenth-century England. The second from Karl Popper’s (1902–94) magnum opus of 1945, making his case for Open Society where creativity and democracy can thrive. The third from six thought leaders of today, illuminating themes of global crisis, social change and reform. Their perspectives (of economist, lawyer, financier, social historian and philosopher) align on the need for new thinking and new foundations of endeavour anchored in the Creative Commons of intellectual property. I also draw on the history of open-source software, supplementary to the discussion of the World Wide Web in Chapter Five.
I then circle back to the care information utility and where it should be pitched in the ecosystem of health care services, alongside the information systems of today. One goal must be to enable the still depended-upon legacy system functions to migrate safely, with the least disruption, into the new organic ecosystem that the information utility will nurture, incrementally, over time. In Chapter Eight and a Half, I described progress towards a central component of the utility, which bridges between knowledge, practice and community. This is the citizen-centred digital care record–its serial non-delivery being the fifty-year-old elephant in the room–perhaps not so old, for elephants!
So how can and should the care information utility be created, maintained and sustained? What is required for implementing and nudging change towards realization of a functioning information utility for health care?
Implementation One–Approach and Method–Learning and Showing How
Implementation is where we learn about wicked problems and how to tackle them. We learn how to do things by doing them–there is no other way. We must be engineers, keeping a close eye on what we are trying to achieve and aware of how the computer may be helping or hindering us in this.8
In science, theory and practice are grounded in hypothesis, experiment and evidence. Creation and innovation arise from left and right field–substantially independently from commentary and prediction. They proceed, like the steam engine, under their own steam and ahead of evidence. My anthropologist colleague in Centre for Health Informatics and Multiprofessional Education (CHIME) at the University College London (UCL), Paul Bate, specialized in the organizational development of health services. He emphasized the need to work from experience of practice into theory of practice, as well as vice-versa, with new ideas–the latter, the traditionally construed ‘bench to bedside’ paradigm of translational medicine. As discussed further, below, this has been called Ostrom’s Law–that is, ‘things that can work in practice, can work in theory as well’!
When formulating and implementing new ideas for tackling wicked problems, what seems often to engender success and sustainable impact is the way in which perceived needs and deficits are tackled. Bate highlighted this in his studies of health care innovations. The way we act can be as important as what we do. We should focus less on theory that predicts, or second-guesses, how the uncertain future emerging from Pandora’s box will play out. We can now predict the weather ahead more accurately and adjust accordingly. But even this knowledge remains couched with increasing uncertainty, the further ahead we look, in days and weeks.
Unfortunately, but inevitably in highly charged realms of politics, innovation as a focus for reinvention and reform is openly or covertly opposed, at times and places where it is most necessary for exposing and helping to clarify problems being faced. With wicked problems, it seems often to be required that anyone seeking a solution be able to demonstrate how to solve the problem before being helped and supported to discover how to do so. As the very wise former head of the Wellcome Trust advised me, thirty years ago, you cannot succeed with this kind of problem by talking and writing about it, you can only succeed by showing how. Until you succeed, no one wielding power will feel able to support you, and when you succeed, everyone will all always, secretly, have been your friend, she said, smiling encouragingly!
Such innovation is about creating and learning by making and doing. It is where head, hand and heart must align. It is mission, insight and alliance. It is not a place where money is easily, if at all, made, other than by the already wealthy, clever or lucky gamblers about the future. Some grab, pre-empt or gamble the future, and some opt out and manage, or prefer, just to gambol into it! Innovative mission is about staying power.
Politicians and civil servants have a hard job in presiding over dreamers, apparatchiks, gamblers and those who gambol. Managers must draw on evidence to focus and lead. But faced with complexity, reasonable concern for evidence can easily segue into treating ‘lack of evidence’ as ‘evidence of lack’. When there is a lack of evidence confirming something, it is often mistakenly treated as untrue. This is a cardinal error in clinical practice as well as a potential Achilles’ heel of ‘closed-world’ logic, as was discussed in Chapter Two. It may not do the health of the nation much good, either. We set standards that evidence must meet and use them as instruments for regulating innovation in areas not yet well-understood, but where there is pressure to frame and manage them, nonetheless. This is more defendable when managing well-established discipline, but of questionable value when charting the unknown. We need to create and experience futures before we can evaluate them sensibly with evidence. Disruptive futures are feared and shot down, for lack of evidence, before they can, or are allowed, to prove themselves. Remember the debunking of Charles Babbage (1791–1871) by George Airy (1801–81), as recounted in Chapter Five! Disruptive innovation was the focus of the economist Clayton Christensen (1952–2020).9
In Chapter Five and elsewhere in the book are numerous stories of obstruction of what ultimately proved successful and important insights and innovations, from centuries ago in the Industrial Revolution and in modern times–James Lighthill’s (1924–98) take-down of AI, for example. Funny from afar but not so funny up close, in similar machinations of the information revolution of today. Failure to marry necessary but inevitably disruptive innovation with enforcement of status quo often betokens hidden or unrecognized issues of understanding and capacity–what Whitehead and King saw as poverty of ideas and pretence of knowledge. King wanted more focus on narrative and storytelling, and my Chapter Eight and a Half tells a story.
Endeavour that sets out to create the care information utility will, inevitably, bring to the fore undecidable aspects of ‘wickedness’ in the problems addressed. Is human society capable of, and up for, the shouldering of the personal responsibilities that are entailed in realizing the personal expectations of health care services in the Information Society? Our expectations of and about other people in our community are easy to express and readily communicated widely in the Information Age–this is a distal connection. Our individual trust and participation in that community will depend on ways available to each of us, to help us feel part of and valued in achieving shared goals–this is a proximal connection. Enhanced distal connection and diminished proximal connection do not fit well together. Will the creation of the care information utility in Globalton10 community run aground, and rougher justice and injustice prevail in health care, by default? Zobaczymy [we will see]!11 The future will be created, one way or another.
There is no logical way to argue such matters of belief, one way or the other–we do not know the answer, or even if there is one, but we do have responsibility and opportunity to work for the creation of the future we want to see. Horses backed and decisions taken, and the outcomes they lead to, one way or another, will matter. These are new times and today’s answers do not lie in retrospective view. Stubborn and obsessed innovators and their innovations look forward and reveal paths ahead of us in the wood. Social movements start in threes and tens and rise to hundreds and tens of thousands. The statistician Lionel Penrose (1898–1972) proposed a square root law to characterize the power of social influence, after studying the voting behaviour of groups.12 I have found this insight helpful in thinking about the strategic growth of openEHR. In seeking to influence a group of people of size n, a cohesive sub-group numbering the square root of n can prevail. Ten committed and coordinated people can influence one hundred–in good and bad directions, of course! You can think of this another way–if you face a problem of scale n, first focus on a goal of scale square root of n–or root(root(n)) etc. to a scale that is tractable–and then work and seek to scale up from there.
The flip side of audacious hope is the resigned pessimism that can easily prevail in the face of the extent of wasted investment and opportunity that has been sunk in and now holds back progress. Much of the current legacy of health information technology (IT) systems is in a slow extinction phase, as indeed is that from much else of the historic investments to date in all IT systems. Globalizing monopolies are hoovering up some of the remains. I have seen and heard trusted reports of what lies under polished ‘car bonnets’, in too many places, not to know this. Many suppliers of systems know it, too, and are in survival or safe exit mode.13
We must not disregard or deny extinction events, including extinction of software technologies or patterns of health care; it is too costly. As with changing a house, there comes a point where modification is too costly and disruptive, and knocking down and starting again is the best and most cost-effective way forward to achieve the new house desired. The in-between stage is hard. We have neighbours two doors up from us, who, for eighteen months, have been creating a new house over the foundations of an old one–the family is living there as it metamorphoses. They have been caught by a delayed timescale, consequential on having started the building work just a couple of months before the Covid-19 virus struck! Shortage of materials, subsequent discovery of weak foundations, woodworm and more, have doubled the estimated construction time to eighteen months and still going. And they work from home and have teenage children! Other neighbours, at the end of the road, with four younger children, decamped to a fortuitously vacant close-by house while their builders moved in, ripped the house apart and rebuilt it. It has all been done in six months.
But we cannot move out of health care information systems and services while we rebuild them! We must work in situ, and this multiplies the complexity immensely. Bringing new imaging systems to a radiology department is almost straightforward, when contrasted with a project for creating and maintaining the integrity and continuity of part-paper, part-electronic health care records. These records cannot continue to be lost, in the ways that they have been multiple times during my career, due to organizations migrating them onto new systems that are not backwardly compatible. Data migration has been so complex that there has often been little choice but to throw up the hands and decide not to try. Data migration between systems lacking shared semantic and syntactic information models is a risky, noise-generating undertaking, if not intractable and unsafe. It makes no sense to continue to pile resources into pretending otherwise or believing new hype, that a new method can magically achieve it, where repeating history has indicated otherwise. This is a good example of one of the Susskind book’s short-term expedients that do long-term harm. Neither should we countenance placing all eggs in one or a few, monopolistic baskets–what one might provocatively describe as a ‘basket case’ strategy!
So, what of implementation of care information utility?
- Align under a simple monicker: A citizen-centred care information utility, perhaps called openCare;
- Tackle tractable goals in support of well-delineated groups of citizens and their supporting professionals, that integrate at home, in hospital and care settings, and on the move within and between countries, in their daily lives;
- Be clear about and pursue purpose and goal in improving the balance, continuity and governance of services;
- Focus on what matters to citizens in their health care services, and to the professionals who serve them;
- Focus on and engage carers and volunteers;
- Focus on services that bridge disciplines and professions across sectors of care;
- Focus on common ground;
- Think and act both locally and globally;
- Adopt an open platform;
- Build and support collaborative teams, environments and communities;
- Build iteratively and incrementally, in individually manageable and beneficial stages;
- Build in parallel and integrate;
- Prioritize Little Data and let the Big Data take care of itself. As Michelle Obama writes in her book The Light We Carry, we must go small before we can think big.14 We should focus on small and completable tasks–that is how we develop and grow.
Approach–the Culture of Care Information Utility
The approach proposed, here, is a natural and logical progression from the fifty-year halfway stage we have reached, as we now look forward to the next fifty years. In parallel with the opening of new vistas of prevention, detection, treatment and management of illness, the utility will reflect the greater capability and personal autonomy of the citizen in understanding and managing their personal health care needs, as an active participant who shares more fully in what is decided and what is done and is owner and sharer of their personal data. This contrasts with past approaches to information systems and their governance that have painted the subjects of care as passive actors, treated implicitly as a source of data to be harvested in pursuit of stuff that is done to and for them. We are at a bifurcation of paths forward in the use of information technology–one on a downhill and increasingly fragmented pathway, patching up inevitably always overburdened services, and one on an uphill and increasingly integrative pathway, building outwards from the individual citizen and their health care needs as a global villager, from their home.
This integrative goal is implicit in the image of the inverted triangles, based on Richard Smith’s landmark BMJ editorial of 1997 (see Figure 7.10) and depicting the transition from Industrial Age medicine to Information Age health care. In this perspective, services will focus and be based much closer to citizens at home. They will own their personal data and have greater personal autonomy and associated rights and responsibilities for taking care of their health. Services supporting them in these matters will focus more locally and around them. It has been a failure of vision of the intervening quarter century that too much attention has focused on advancing and shoring up struggling institutions and the data silos of fragmenting and overloaded Industrial Age medicine and social care, and too little on creating new, both real and virtual, environments for the delivery of health care services, in keeping with changing science and society.
This change of approach to care information systems will reflect and represent a transition of values and principles, extending throughout many communities of interest concerned with health and wellness in society. The lesson of experience of wicked problems like this is that it is impractical to orchestrate such a transition and inadvisable to leave matters to individual sectors or free markets to organize. It requires inclusive enablement of communities of interest, environments and endeavours. The multiplicity of potential connections embraced by such wide-ranging communities of interest is immense and realizing the vision can but be tackled collaboratively. There are many and diverse resources that the care information utility can draw on and contribute to. Again, incremental development and prioritization are inevitable. As with the Good European Health Record (GEHR) project described in Chapter Eight and a Half, the mission to imagine and create an architecture of this information utility is once more an iterative and experimental process that should be conducted in the public domain. What are the requirements and how can these be expressed in terms of an information architecture? This work is at the same early stage that I described in Chapter Eight and a Half, when writing about the workplan and drawing together of the GEHR project requirements. GEHR started from an existing prototype architecture and incremented from this in successive stages of modelling, implementation, testing and scaling. openCare can build from where openEHR has reached, and engage community-wide teams and organizations, aligned around shared goals, methods and governance. It can create and test prototypes and evolve iteratively and incrementally from there.
In tackling the wider integration of health and wellness services, the Nordic Countries stand out as pioneers in the formulation and implementation of their plans for the health and social care domain, with individual populations of Finland, Norway and Denmark, of around five million citizens, Sweden around ten million and the other smaller countries bringing the total to around twenty-eight million.15 The initiatives for Finland provide an instructive example, where the openEHR industry partner Tietoevry is playing a coordinating role in the creation of supporting information systems.
In 2022, the country has embarked on a complete reorientation of the organization of health care, social welfare and rescue services. In February 2022, presentations were given to a Nordic Countries meeting to consider collaboration in openEHR implementation. The aim of the proposed reform was to offer the population more equal access to services, to reduce disparities in health and wellbeing and restrain costs. In the IT dimension, focus was placed on service coordination, integrated health care and social welfare services and well-managed care paths, digital services and digitalization of processes. There will be considerable organizational transformation over the coming year, to create a national network of twenty-one Wellbeing Counties plus Helsinki and Åland, for organizing health care, social welfare and rescue services. Funding of the counties will principally be based on central government funding. This is a shift from services based on one hundred and sixty primary health care centres and twenty-one central hospitals, five of which are university hospitals; and from a previous configuration of two hundred and ninety social care units and twenty-two rescue departments managed by municipalities. Some two hundred thousand people will have a new employer.
This is not a scope as revolutionary as that implied by the Richard Smith diagram, but it is an important stepping-stone in that direction, tackling the re-integration of ‘health care and social welfare’ services, drawn together around a common methodology for standardizing care records. To my way of thinking about the implementation challenge of an information utility architecture that builds outwards from the citizen, there will be a requirement for wider integration with all manner of other products, activities and services that help promote individual wellness. Help in coping with and monitoring chronic disease; exercise and nutrition; social prescribing–for counselling and support of mental wellbeing, for example; personal advocacy and support services; citizen-based networks reporting on experience of, and coping with, disease. These all connect within the citizen’s purview of what is involved in keeping well and coping with illness. There is a huge network of home-based carers, hospice and other voluntary-sector support services, and local and national charities that contribute. Although not all within the scope of national government funding, they may attract large amounts of local government funding and public donations. This is where a locally framed and governed utility could be highly beneficial, by encouraging and facilitating local community ownership of needs and coordinating collaborative endeavours in concert with taxation-funded services.
I draw, below, on ideas gained in working for many years to support the StartHere charity, founded by Sarah Hamilton-Fairley and her husband Richard Crofton. This was inspirational and influential work, lauded and successful in multiple pilot projects, but ultimately not something that disparate community interests were prepared to risk their separate interests and identities to sustain. It lacked the care records dimension and my thoughts on integrating these under a common framework of global and local governance led to the conception of the care information utility I propose here.
All this will come to the fore in tackling health inequalities and shifting the focus of care onto a worldview of the citizen in need, not the organization providing services. It needs fresh thinking inclusive of this wider community of interest. It needs reinvention and redefinition of scope of service and articulation of requirements addressed. It needs new focus on wellness and the citizen at home. Citizen and service focus are complementary. We will need to overlay wider and complementary perspectives onto the ellipses of the GEHR requirements for comprehensiveness of care record architecture depicted in Chapter Eight and a Half (see Figure 8.21): wellness and illness; patient and professional; citizen and community; local and global standards and governance; citizen and academic science; computer science student and professional system developer.
At this point and time, as described at the beginning of Chapter Eight, we appear to be at a Robert Frost moment of choice between bifurcating pathways in the wood. Up-down and down-up paths beckon. Along the down-up route there must be vision and principle for connection of people, community, environment, architecture, design, resource, organization and governance. There must be a trusted and shared purpose and goal, forming the basis of cooperation. There must also be a process or roadmap that connects and creates from the here and now and its legacy, to a new and more sustainable future legacy. There must be incremental steps, and learning along the way, spreading out and integrating, horizontally across landscape of disciplines, professions, services and countries, and vertically within governance and government. As is being more widely spoken of, now, this is reinvention more than reform of health care. The care information utility will be one thread in the braid of that reinvention.
The technical dimensions of the reinvention will require authority within political, professional, commercial and institutional circles; the social dimensions will require authority within personal and community circles. Authority is not conferred–it is acquired. None of this can be mandated or imposed–it must be seeded, nurtured and helped to grow. There must be practical credibility, of head, hand and heart, throughout. These are the dimensions of the challenge for health care services to come through their anarchic Information Age transition, facing up to current fragmentation and inequitable unravelling of service, infrastructure, discipline and profession, and the need for their reinvention, reform and reassembly, supported by an inclusive, integrated and whole care information utility.
This rather ethereal vision of the implementation challenges posed by the utility is, admittedly, an abstract and symbolic one, and it sits alongside other symbols whereby people and communities gain strength and trust, to cope and cooperate. As Robert Axelrod wrote in The Evolution of Cooperation, based on his influential research in the early 1980s, trust is the foundation of human cooperation.16 Whitehead’s warning that I have quoted in the book’s Introduction, and again in the Postscript, also resonates–society must learn how to sustain its symbols or risk its own destruction by the anarchic forces of fundamental change. The Information Age is a transitional era of fundamental change in society. To borrow, and possibly misuse, a phrase from Benjamin Franklin (1706–90), ‘We must all hang together, or assuredly we shall all hang separately’.17
The practical things needed to achieve the specific goals we set out towards creating the care information utility can all be made and done incrementally, over time. In development of human life, the embryo evolves a very long way towards wholeness, from single cell to body, before it is born into the world outside. Care information utility already has a living body, personality and community. It is directly relevant to the here and now of policy and practice for health care information. And crucially, it has examples that support and evidence it, and growing influence at a global scale: in Australia, Brazil. China, England, Finland, Germany, India, Italy, Jamaica, Japan, Netherlands, Norway, Pakistan, Portugal, Russia, Scotland, Slovenia, South Africa, South America, Spain, Sweden, Uruguay, Wales and many more, too extensive to list or possibly not yet known about.
When I first met Xudong Lu from Zhejiang University in China, while representing openEHR in Sao Paulo at the 2015 Medinfo world conference of Medical Informatics, he presented an astonishing paper about implementation of an openEHR-based health record system at his nearby two-thousand-bed hospital. He had built a team and created this system solely from the Creative Commons specifications of the openEHR architecture of electronic health records and the then existing, and now hugely more comprehensive and refined, body of clinically curated openEHR models of clinical data–the largest such repository in the world and in large part a product of cooperating professional volunteers, across disciplines, professions, organizations and industries.
And today, people all over the world can download and spin into life a functioning open-source OpenEyes ophthalmology record keeping system, the same as that now servicing approaching fifty percent of eye consultation records across the UK. And openEHR and OpenEyes are incrementally being harmonized, for national platforms of care record services, in whole national jurisdictions. The achievement of incremental goals, contributing towards the realization of Care Information Utility (CIU) is happening, now, North and South in the world. It started, as most seeds do, with a very small chance of success–it is now a 50:50. We are halfway there–the theme of the Postscript–echoes of Bon Jovi!
Having gone on at length about the importance of practical implementation, as is my wont, I now look back into history, as is also my wont, to the origins of two phrases–the Creative Commons and the Open Society.
The Commons
The word ‘common’ is semantically rich. It is the common land on which we can all walk, and maybe graze our horse. It is common sense, which is, paradoxically, both easy to talk and argue about and nigh-on impossible to define from an algorithmic and data-driven perspective, or have AI acquire! It is social and intellectual rank–House of Commons and House of Lords in the UK Parliament; scholars, exhibitioners and commoners in the archaic Oxbridge student parlance of my days there.
Common land was an interest of the historian Richard Tawney (1880–1962). After graduating from the University of Oxford in 1903, he and his friend William Beveridge (1879–1963) lived at Toynbee Hall, then the home of the recently formed Workers’ Educational Association. Tawney is a hero of the widely read and listened to Harvard University philosopher, Michael Sandel, who recently published his own critique of contemporary society, entitled Tyranny of Merit.18 In medieval England, there was a balance of land divided into strips, where villagers looked to their own needs for cultivation, and common land that was shared. This was an expression of the public and the personal, of owning and sharing. And in this environment, there was trust and continuity, independence and mutuality in life. This spirit is also expressed and illustrated today in the concept of Creative Commons. One must not get too starry eyed–there is always unfairness, poverty, criminality and exploitation, as well. But common ground was a valued and valuable resource. And in the Enclosure Acts of early nineteenth-century England, common land was enclosed and privatized, thereby destroying habitat, life and an enduring culture of community and countryside. John Clare (1793–1864) described ‘Enclosure like a Bonaparte let not a thing remain’.19 His poetry, nurtured in the rural idyll of his daily life, conveys sensitivity to the importance of this balance of personal and shared, private and public. He expressed this through everyday scenes and features of the landscape–an iconic elm tree–and the history and meaning they embodied.
Some have written of the ‘tragedy of the commons’, others of its ‘comedy’. In the tragedy, individual self-interest exploits the commons and triumphs over collective interest in sustaining and preserving it. In this scenario, as described by Garrett Hardin (1915–2003) in 1968, a group of shepherds graze sheep on common-land pasture; one shepherd places more than their equitable number of sheep, to their own benefit but to the disbenefit of their community of colleagues who keep to their quota. The value of the common pasture becomes impoverished for all, save for the miscreant, for whom default pays off. That is, until the members of the community, one by one, lose heart and the common pasture is no more. The ‘comedy of the commons’ describes how people contribute property and value accrues from its wider sharing. In the Information Age, what is contributed is knowledge and content–not for personal gain but for the good of the community. Examples often cited of this are free and open-source resources such as Wikipedia, and the many open-source projects made public through GitHub, parented by Microsoft, rather as UCL parented openEHR and the Apperta Foundation now parents OpenEyes.
The modern-day Creative Commons is an important and adventurous idea, being played out on common ground. Its legal foundations are tuned to different ways allowed for sharing and building on this common property, in balance with privately enclosed property. It is concerned with protecting and sustaining intellectual property for the common good, and preserving and sharing its value and meaning, for everyone. It is both lodestone and stepping-stone in the quest for social equity. Creative Commons is finding ways to protect and share intellectual property, that do not involve enclosure and defence against access. Lodestones are natural magnets; they naturally align to attract and cohere, and, otherwise aligned, they repel. Stepping-stones show a path across a stream. Thus it is with Creative Commons; we need to explore and understand the opportunities, polarities and forces in play, in shaping and sharing common ground, for the common good.
Common sense comes into play as much through perception of its absence in human thoughts and behaviours, as its presence. Maurits Escher (1898–1972) tackled the challenge of making sense and nonsense from incompatible, inconsistent or intractable ideas, in his collection of iconic lithograph designs, that I have pointed to in several parts of the book. To be valuable as common ground, there must be discipline in the intellectual commons, and a transparent and open balance of theory and practice. Where this balance is attempted on enclosed and opaque ground, it fosters division, exclusivity, inequality and extremity. Information Age infrastructure and services have evolved and migrated onto considerable mutual common ground, as I explore further later in the chapter. Next, I will briefly trace historical ideas about ‘openness’. This is a different trajectory, but the two come together in the context of future information utility.
The Open Society
The word ‘open’ is also semantically rich. Open, ajar and closed doors; open and closed minds; open and shut cases in law, where legal principle and precedent brook no argument as to the outcome; open sesame where anything goes. Open books are transparent–what lies inside is seen. Black boxes hide what lies inside. Black holes presented an information paradox–was information conserved or lost, and how? I gather that there are seven theories at least that seek to resolve this matter! Zobaczymy–or maybe we will not see!
It feels appropriate to mention Popper’s epic book, The Open Society.20 It is a heartfelt account, written while living in New Zealand. The country’s geographical isolation helped it to avoid the spread of world wars from Europe, in the decades in which Popper developed the philosophical ideas set out in the book. Popper went there as an exile from the Anschluss annexation of Austria, in 1938, and the book first appeared in 1945, the year of my birth. New Zealand was a relatively isolated enclave from Covid-19, avoiding the first waves of the pandemic.
The book is long (seven hundred and fifty-five pages) and outspoken. Maybe that is why Bertrand Russell (1872–1970) liked it so much! In my editions, Russell pips Popper in page count–eight hundred and forty-two pages of his History of Western Philosophy, but Popper out-pips Russell with rhetorical invective, decrying culture of deference and centralism leading to totalitarianism. Popper’s highly influential book is an often-florid expression and interpretation of culture, history and belief, born of powerful personal experience. He recognized this in prefacing a later edition, saying it had not been a time to mince words.
Popper had an affinity with Communism after the First World War but in time espoused liberal democracy. He railed against the mirror phenotypes of fascism and totalitarianism exhibited in his growing years. His analysis traced these cultural trends to pillars of Greek philosophy and onward into the twentieth century, sparking fiery debate and accusations of misunderstanding and misrepresentation. A bit like contemporary debates about ontology! His portrayal of the philosophy of Socrates (470 BCE–399 BCE), Plato (c. 428 BCE–348 BCE) and Aristotle (384 BCE–322 BCE) in support of his arguments was criticized, as was his critique of twentieth-century Marxist interpretations of history. He attracted warm support from radical philosophers of the time, such as Ernst Gombrich (1909–2001) and Gilbert Ryle (1900–76), as well as Russell.
Popper also railed against historicism–teleology in historical narrative–maintaining that history was influenced by growth in knowledge, which was inevitably unpredictable. His writings on conjecture and refutation became a key plank in the philosophy of science. I will leave the philosophical debate to others who know how to argue about such matters. My only reason for detouring through this history is to make a parallel with the meaning of ‘open’ in contemporary debate about Information Society, where information technology has become a stepping-stone on pathways both to enlightenment and to monopoly and extremism. The landscape of health care IT is an archaeological record, bestrewn with the remnants of ideas pursued with unsustainable methods, by unsuited and poorly led people, in the wrong place at the wrong time. We need a sense of what constitute open alternatives with better chances for success. A utility centred on proprietary knowledge and intellectual property, placed in control of citizens’ personal data, is most unlikely to prove a sustainable or acceptable model for a care information utility, although both public and private components assuredly will and should feature.
Threads in a Braid
Many threads are being woven together in discussions of major challenges the world faces at the outset of the twenty-first century. Braiding hair can help it to grow faster and provide a more stable structure. Unravelling of braids can lead to a tousled tangle. Transition in society is the disheveled unravelling of braids and the purposeful weaving of new ones. It is also the cycle of downswing and upswing in social cohesion, described by Robert Putnam in his 2020 book Upswing,21 and the similar optimism of Thomas Piketty in his equally magisterial 2022 book A Brief History of Equality.22 The six threads I describe, here, come under headings of economics of property, nature of professionalism, global community, global crisis, pendulum of change and social equality. They have profound implications for creation of care information utility.
Elinor Ostrom on the Economics of the Commons and Property Law
The Nobel Laureate Elinor Ostrom (1933–2012) challenged the assumptions about property that underpin economic theory, especially that which is held in the commons. She analyzed alternative ways of looking at examples of functioning common property, showing how they worked in practice and arguing that if they worked in practice, there must be a common theory to account for their success. This became known as Ostrom’s Law, which Lee Anne Fennell summarized as: ‘A resource arrangement that works in practice can work in theory’.23 I think of the development of openEHR and OpenEyes, with their emphasis on the primary importance of implementation experience, a bit like that!
We hear a great deal about intellectual property and its protection and appropriation for commercial benefit. We hear that the Amazon Company is valued at trillions of dollars while the Amazon rain forest is registered nowhere as a financial asset. For many house owners in South East England, personal property has for many years been accumulating more value in a year than is earned in full-time employment.
Richard and Daniel Susskind on Professional and Personal Sharing of Knowledge
In their book that I discussed in Chapter Eight, Richard and Daniel Susskind concluded that the societal contract–they called it a Grand Bargain–underpinning the relationship of trust between professional and citizen could only come into balance in the changing dynamic of the Internet age if communities and partnerships between communities shared their knowledge. In their seventh chapter, entitled ‘After the Professions’, they dissected the arguments both in favour of and in opposition to the idea of this operating as a Creative Commons, in terms of motivation, incentive, and sustainability. Citing the example of the success of Wikipedia, they highlighted that as a cost-free, supporter-funded initiative, it overcame problems of exclusivity.24 In their envisaged ecosystem, with the sharing of knowledge transacted and governed in the commons, they argued that a new, more equitable and beneficial professional relationship would emerge, trusted on all sides–a Wikipedia of professional practice.
They were not focused exclusively on the professions of health care, but their wider review of many professions provides a useful context for thinking about health care professionalism. It is a mistake to think along the lines often encountered, that because something is different, it is completely different. It seldom is, and such thinking says more about protectionism than the potential for collaboration around common purpose. Health and care have much common ground, with one another and with other professions.
Cass Sunstein on Aggregation of Knowledge and Markets, Deliberation of the Crowd and the Nudging of Behaviour
Cass Sunstein is a Harvard Law Professor who has made extensive studies of group dynamics in the Internet and social media age. In his 2006 book, Infotopia, and others of his works, he reflects on the many new contexts and communities in which we now accumulate and share knowledge and reach decisions, both individually and in groups debating with one another.25 The rise of the Internet has changed market mechanisms and Sunstein explores the new ways in which these can be predicted and gamed, and how they interact to cajole and persuade, through new forms of targeted advertising and manipulative manoeuvres that seek to influence and exploit behaviour.
He considers emerging Internet resources and tools, such as open-source software, wikis and Wikipedia, and revisits citizen rights in this context, settling around traditional areas of education, shelter and health, and with new focus on protection against monopolistic practices. He is concerned by the potential for the weakening of democracy through retreat into echo chambers of views and experiences that play out online, and isolated from direct human contact and ideas that might challenge their beliefs–a process called ‘cyberbalkanization’.
In 2021, Sunstein teamed up with Daniel Kahneman and Olivier Sibony, to publish Noise.26 This book draws on Kahneman’s ideas about behavioural economics, set out in his celebrated book, Thinking, Fast and Slow, showing how we are all influenced in our decision making.27 It presents a new and more forensic appraisal of how human judgements exhibit different kinds of noise and bias, including, for example, in sentencing practice of judges and clinical judgement of doctors.
Mark Carney on Global Crisis of Money, Climate and Pandemic
In December 2020, the annual BBC Reith Lectures were delivered over the Internet by King’s successor as Governor of the Bank of England, Mark Carney. Anticipating his new role as United Nations (UN) Coordinator of Policy on global climate change, he drew parallels from three crises of our age, and common problems of economics and society that run through them. These were the near collapse of the world monetary system in 2007–08, the escalating climate crisis and the 2020 viral pandemic. The lectures reminded me of John Houghton’s (1931–2020) much quoted remark, in relation to his time working on the UN International Panel on Climate Change initiative, decades ago, that humankind only takes issues seriously when in crisis.
Carney identified three areas of focus for change: engineering, politics and finance (new opportunity in innovation). His focus was on barriers to change, and he noted that the Gates Foundation emphasized the significance of speed and scale in their initiatives; policy must be driven quickly to scale, if it is to succeed.28 Agreeing a common approach and making it a reality should be as high a priority as dotting i’s and crossing t’s in selecting the particular policy to be implemented.29
In his lectures, Carney highlighted Cass Sunstein’s above discussed work on how social movements gain traction. He set out some principles of implementation of change, based on feedback and self-reinforcement cycles, with ‘values driving values’. Nothing succeeds like success, as it were. His emphasis was first on ‘reporting’, citing the maxim that what gets measured gets managed. His second focus was on risk management–all sectors must align around risk. His final emphasis was on what he called ‘returns’–making innovation for sustainability a business and making investors hold company policies and plans to account around specific values that their work embodied. This idea aligns closely with what Tett described in Anthro-Vision, as mentioned above, as the changing emphasis towards goals of sustainability which she had noted at the Davos conferences of world corporate leaders she had attended and reported on.
Carney’s take-home message in his Reith Lectures was the need to tie policy to what he called the leverage of social coalitions, with fairness, and income and welfare reflecting values. Again, this seems much in tune with Tett’s anthropological perspective, as well as with the ideas set out by Mariana Mazzucato in The Entrepreneurial State, when discussing reformulation of economic relationships in the world economy, in response to the crisis of VUCA.30 These ideas are much in keeping with the purpose and goals of care information utility, as proposed in this book. Carney’s central idea of values driving values is also descriptive of practitioner peer group review and reinforcement, on the ground. This bottom-up perspective and approach needs equal status alongside a managerial approach that takes a top-down view–both are seeking to ‘drive’ improvement of quality of services, and both are needed if a care information utility is to be created and sustained.
Robert Putnam on Upswing
As referred to several times in the context of previous chapters, this is a forensically researched and well-illustrated account of the half century or so ‘upswing’ of society from 1900 in the USA–from ‘I’ to ‘we’, as Putnam characterizes the era–with its emphasis on concern for the common good supplanting a culture of individualism and social divisiveness. The following half-century or so of ‘downswing’, from the 1960s onwards, he characterizes as ‘we’ back to ‘I’, with emphasis on assertion of individual rights and cumulative pressure on countering social and group norms that had come to frustrate individual freedoms. Putnam is four years older than me and has lived through downswing. His copious and wide-ranging socio-economic data analyses, notably including those on gender and race, are authoritative in tracking the century of American history, through which my parents lived, here in the UK.
Graph after graph of Putnam’s social and demographic analysis exhibits a similar inverted U-shaped curve of upswing and downswing over the century. One cannot help noting that the Information Age has emerged alongside these fifty years of downswing. Putnam does not connect the two, but it is tempting to postulate a causative and not purely associative relationship with the local social disconnects and global virtual connects of those times–one wonders!
In thinking of the prospects for the coming decades of the twenty-first century as we emerge towards the Information Society, with the experience of VUCA and related ESG priorities and calls for new focus, it is interesting to note Putnam’s optimism. He writes that the historical perspective laid out in the book leaves him more optimistic than he has ever been about the future trajectory of American society. Let us hope so–for other countries, too.
Thomas Piketty on Equality
As I completed my second draft of this book, around April 2022, Piketty’s Brief History of Equality appeared. It is itself a woven braid of decades of his treatises on the theme of equality in society, written in French and translated to English in this inspiring book. To do it justice briefly, here, is well beyond my ability, but I have collected a set of quotations from the introductory and concluding sections, where he sets out his stall. I have abbreviated them to exclude their particular contexts, simply to highlight their general relevance and connection to themes of this book.
From the book cover:
We need to resist historical amnesia and the temptations of cultural separatism and intellectual compartmentalization. At stake is the quality of life for billions of people. We know we can do better. The past shows us how. The future is up to us.
Regarding knowledge and learning, Picketty writes:
The process of collective learning about […] is often weakened by historical amnesia, intellectual nationalism, and the compartmentalization of knowledge. In order to continue the advance […], we must return to the lessons of history and transcend national and disciplinary borders.31
Regarding transition:
[…] economic and financial crises often serve as turning points where social conflicts are crystallised and power relationships are redefined.32
Regarding instability and iteration:
However, each of these arrangements, far from having reached a complete and consensual form, is connected with a precarious, unstable, and temporary compromise, in perpetual redefinition and emerging from specific social conflicts and mobilizations, interrupted bifurcations, and particular historical moments. They all suffer from multiple insufficiencies and must be constantly rethought, supplemented, and replaced by others.33
Regarding social and organizational change:
The social sciences naturally have a role to play in this, a significant role, but one that must not be exaggerated: the processes of social adaptation are the most important. This adaptation also involves collective organisations, whose forms themselves remain to be in reinvented.34
Regarding pitfalls between theory and practice:
Two symmetrical pitfalls must be avoided: one consists in neglecting the role of struggles and power relationships […]. The other consists, on the contrary, in sanctifying and neglecting the importance of political and institutional outcomes along with the role of ideas and ideologies in their elaboration. Resistance by elites is an ineluctable reality today, in a world in which transnational billionaires are richer than states.35
Regarding the process of reform:
Questions regarding the organisation of the welfare state, […] are both complex and technical and can be overcome only through a recourse to history, the diffusion of knowledge, deliberation, and confrontation among differing viewpoints.36
Regarding a balance of politics and ideas:
It is not always easy to find a balanced position between these two points: if we over emphasize power relationships and struggles, we can be accused of […] neglecting the question of ideas and content; conversely, by focusing attention on the [theoretical and programmatic weaknesses of ideas and content] we can be suspected of further weakening [them] and underestimating the dominant classes’ ability to resist and their short-sighted egoism (which is however often patent).37
Regarding the importance of an empowered citizenry:
[such] questions are too important to be left to a small class of specialists and managers. Citizens’ reappropriation of this knowledge is an essential stage in the transformation of […] relationships.38
And finally, in his conclusion, Picketty advocates for the reframing and reorganizing of common ground:
We must also describe precisely the transnational assemblies that would ideally be entrusted with global public goods and common policies […] Economic questions are too important to be left to others. Citizens’ reappropriation of this knowledge is an essential stage in the battle for equality.39
There is much of the culture and values of care information utility woven into Piketty’s vision, as extracted, and summarized here.
Co-Creation of Common Ground
This book is about the co-creation of common ground on which to base a care information utility, and discusses achievements to date as stepping-stones to that end. It is about what we grow there, and how we live and work there. The previous section drew together diverse perspectives on what implementation on common ground entails and how these complement one another. It is where those seeking to fulfil and achieve shared purposes and goals, combining diverse threads and methods of implementation, come together to complement, collaborate and co-create, thereby braiding and strengthening their endeavours. It is another organic analogy. Braiding occurs naturally in plants. The urgent new shoots of honeysuckle and wisteria outside my study window flail independently as they grow, seeking traction. They find one another, intertwine as a braid, and grow upward, stronger. In relation to the braiding of the many threads and methods of care information utility, in what contexts, according to what principles and governance, can they be created, extend to scale and be sustained?
In tackling grand challenges with wide-reaching impacts, from the local to the global, the balance and alliance of public and private sector endeavour is crucial. Where such alliance is scarce and balance questionable, their impact can be harmful. Reinvention of the balance and alliance of the two sectors requires new ideas, as Mazzucato has explored.40 For care information utility, these ideas must reflect and respect a shared common ground of values, principles, goals and methods. Fred Sanger (1918–2013) worked always in the public domain. James Black (1924–2010), John Vane (1927–2004) and Salvador Moncada, whose paths crossed with mine at various times, worked in partnerships of public and private endeavour. Great scientists such as these created, underpinned and led molecular biology and pharmaceutical science for several decades. Global money and industry organized, scaled, monetized and further developed its products and markets. In like manner, academic research created, underpinned and led methods for coping with large-scale unstructured data, and these foundations have been built on in the global tech companies of today.
Modern-day pharmaceutical industries have grown from intellectual property created and shared in academic and health care environments. Government, philanthropy, industrial partnership and individual voluntary and charitable endeavours have co-created and sustained those environments. AI, automation and robotics have been similar in provenance. No parties acting alone could have made this progress. Google and Facebook have grown from and traded on knowledge created on common ground, appropriated into private enclosure, aided by passive data volunteers. Wikipedia builds in the public domain, on the contributions of an active community of volunteers who offer their knowledge; it is a utility that can grow, enhance and share their knowledge and resource. In the Information Age, models of public interest have faced powerful competition with business models of enclosure. The Creative Commons is powering a reversal of that trend and enabling new and more open business models to prosper.
The word open has found a new niche in the Information Age–open-source software, open data, open knowledge–even openEHR and OpenEyes! Being ‘open’ does not in itself solve any wicked problem and it raises new problems of viability and governance of its own. As an expression of human aspiration and commitment, it is a bugle call and flag to rally under, about culture and practice of the Information Age. It is interesting that in the connected contexts of the previous section, several of the cited authors make connections with the advance of the open-source software movement, and with Wikipedia, as pioneering initiatives in creating common ground.
Open-source Software
A good starting point, here, is the story of Unix. Quite early along my software songline, I became aware that manufacturers’ operating systems for their computers were an eclectic mix, difficult to get to grips with and work with, and consuming a good deal of time, effort and resource on the part of their users. And this was ephemeral knowhow–one got better at it as one tackled essentially the same challenges for successive machines that one used. But it tended to ensconce tribal loyalty to particular manufacturers and their ways of doing things, as the devil one knew. People built their careers around International Business Machines (IBM), Honeywell, International Computers and Tabulators (ICT), Digital Equipment Corporation (DEC), Data General, Hewlett-Packard… and so on.
The idea of the AT&T Unix operating system emerged in the Bell Labs research centre. It was to be portable across different computers and provide a common programmer and user experience of a multitasking, multiuser operating system. Ken Thompson and Dennis Ritchie were its originators at Bell Labs, and the system was licensed from there, not originally as open source (i.e., providing all the code to its users), but addressing many of the needs for a common research computing environment. It spread under its own momentum across the world. From this beginning in the 1970s, arose a Unix family of implementations on different machines.
In 1991, the Finnish Computer Scientist Linus Torvalds published the first version of an open-source Unix-like operating system, which was named Linux–a bit of Linus and a bit of Unix! The license chosen was a cautious one, to preclude downstream meddling that might corrupt the free dissemination and functional integrity of the standard version. Torvalds was and remains the Fred Brooks style of architect–in charge, capable and motivated. New business models emerged for companies providing installation, training and consultancy services based on Linux, which remained free to download and unrestricted in use.
In the following decade, the Android open-source project drew together a community of developers to create an operating system that spanned smartphones and notepads. From 2005, it was taken in and run by Google, which set and maintained a high standard for cost and performance, with the software freely downloadable under the liberally permissive Apache 2 open-source license. The viability of this software ecosystem depends on Android remaining state of the art, such that there is no functional or cost incentive for forked versions of the code to emerge, although these are technically permitted under the license. Google, itself, mixes proprietary code with Android open-source code in its own products, presumably to maintain some exclusivity. Other suppliers can do likewise.
In the openEHR world, as described in Chapter Eight and a Half, open-source versions of the openEHR platform have germinated and grown. The first seedling was the Opereffa initiative, a collaborative effort between my student Seref Arikan and myself, for which we further teamed up with Tony Shannon, then a Leeds-based clinician in the UK and now a health IT leader in Ireland. Tony, in turn, pioneered his EtherCIS initiative and, in parallel, Pablo Pazos, a computer scientist in Uruguay, pioneered his EHRServer open platform. These pioneers and threads have now braided together in the EHRBase platform initiative, spearheaded by the strong and resilient Vita Group company in Germany, which is attracting national funding there and worldwide interest and adoption.
As with Unix, Linux and Android, this progressive commoditization of an open-source and standardized platform for openEHR is creating new common ground. This is enabling greater mutual understanding and alliance among clinical, technical and organizational users and developers of openEHR-based systems, and lowering the bar, economically and timewise, for development of new, mutually coherent and innovative applications. What would, many years ago, have consumed a large part of any project budget, for creating a machine operating environment for the planned new application, is now available as common ground, downloadable to a local machine or operable on globally networked infrastructures and services, such as Microsoft Azure, Amazon Web Services, Google Cloud and IBM Cloud Resources.
The software of applications is now configured in layers of a program stack. These layers integrate with one another and may bring in products and services from different software suppliers. They intercommunicate through standardized interfaces between each stack layer, to build the complete platform required for the application to run. Programmers specialize in different stack architectures that support different kinds of application–a web service, a database service, a geographical information system and so on. Wikipedia lists some thirty such available generic software stacks.
Bench chemistry evolved in a similar fashion, connecting resources and processes in a chain of chemical reactions, increasingly operating and connecting them automatically. Chemists and life scientists evolved the different stages of the underlying chemical analysis and standardized their interfaces. This incremental process is now mirrored by a series of robotic devices positioned along an automated production line. Each robot collects the product thus far assembled by its predecessors and additional materials required for the assembly tasks that it, in turn, is delegated to perform. It completes this next stage of subassembly and passes the incrementally assembling product as input to the following stage of robotic assembly along the line, and so on until the final product has been made.
What, though, if people like Sydney Brenner (1927–2019), Fred Sanger (1918–2013), Max Perutz (1914–2002), Francis Crick (1916–2004), John Sulston (1942–2018), Paul Nurse and many others had patented the interconnecting life science knowledge and knowhow they had ‘assembled’, on which the industrial automation of genomic medicine has been built? There would be no biotech industry–just entrenched biotech monopoly and probably one of considerably less sustainable utility for the world. IT system suppliers have, carefully and selectively, set out to enclose and protect the methods and interfaces that make them special and able to control their proprietary platforms. Let us hope that the tech giants of today find other planetary and interplanetary ambitions on which to compete and choose to adopt a more collaborative approach in their interface with a care information utility.
The story of my encounter with the open-source platform, DOSBox, in reviving legacy work on the Mac Series of Physiological Models, which I tackled alongside writing Chapter Four of this book, and recorded there, is another example of open-source community development encountered along my songline. I have come across others–sharing methods of image processing for example. We are still learning, experimentally, where open-source principles and practice will fit in the co-creation of care information utility. From my perspective, what constitutes common ground of this collaboration must, by definition, be transparently owned, shared and governed in that spirit. That is not to say that proprietary property and methodology cannot and will not play crucial roles. It does, though, say that success in achieving balance, continuity and governance of care services will depend on what is held in common within the care information utility.
Method–Discovering the Form and Function of the Care Information Utility
‘Just the place for a Snark!’ the Bellman cried,
As he landed his crew with care;
Supporting each man on the top of the tide
By a finger entwined in his hair.
‘Just the place for a Snark! I have said it twice:
That alone should encourage the crew.
Just the place for a Snark! I have said it thrice:
What I tell you three times is true’.41
I have placed emphasis on the importance of ‘implementation, implementation, implementation’ three times in Part One of the book. It must be triply true! We can only discover the form and function of the care information utility by imagining and implementing it. It was my mum who introduced us children to this whimsical and insightful poem. It often seems to be our streetwise mothers who best combine those essential attributes of whimsy and insight in our lives!
Lewis Carroll’s (1832–98) Snark poem is sometimes described as an allegory of the pursuit of happiness. According to the poem, elusive comforting and benign Snarks sometimes turn out to be malign or harmful Boojums. In context of this book, the poem might be an allegory of the pursuit of AI in furtherance of Eric Topol’s ‘Deep Medicine’.42 Will AI prove Snark or Boojum, there? Or it might be that the hunt for the care information utility, as Snark, leads to a noisy and biased Boojum, not much better than the disjoint silos of knowledge and data today–we must track both these Snarks carefully!
I made my first attempt to picture the care information utility (see Figure 9.3) ten years ago, when closely involved in the StartHere initiative that I describe later in the chapter. It is a concept still in embryo.
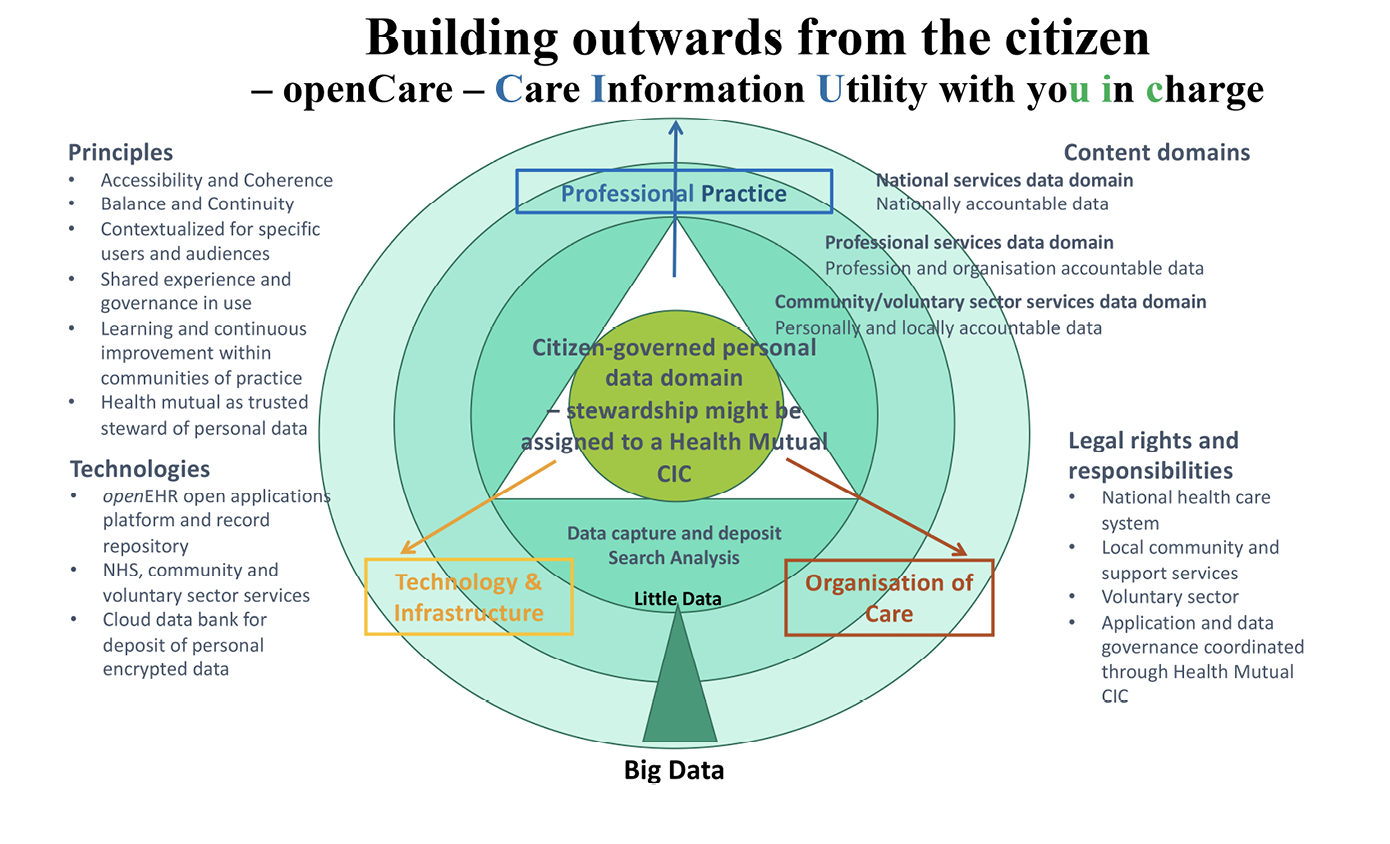
Fig. 9.3 A first step towards framing a scope and architecture of requirements for a Care Information Utility, with you in charge–CIU with uic! Image created by David Ingram (2012), CC BY-NC.
In thinking about the multiple facets shaping and reflecting form and function of this care information utility, my geometrically inclined (and maybe also annoyingly alliterative!) mind constructed tables of what I loosely, and probably somewhat inconsistently, described as monads, dualisms or dichotomies and tripods or trifectas. The monads are seen as values and principles–things on which we need to find agreement. The dualisms are sometimes seen as alternative realities but often as usefully complementary ideas–things that we need to balance and broker between. In the Introduction, I discussed Robert Oppenheimer’s 1953 BBC Reith Lectures, in which he used particle and wave duality in physics to illustrate general points about the importance of dualisms, or complementarities, in shaping our ideas. The dichotomies are sharp cuts or divisions, seen as contrasting, competing or opposite perspectives. False dichotomy is sometimes used as a device to divide and control, for purposes other than clarification of truth.43 The tripods are groupings that mutually reinforce and cohere, stably, in defining and building an architecture–the term draws an analogy with stable physical structures. The trifectas relate to matters where all three components are needed and mutually complement one another (for example ‘the trifecta of life’: self, work and relationships). It originated in discussions of gambling outcomes (as a term for a horse-racing bet in which the first, second and third place finishers are chosen in the correct order), but has since broadened in meaning to refer to a group of three.
Figure 9.3 and the following two Tables are not intended as in any way polished–they build on and give another take on the values and principles that guide and frame implementation, as set out at the end of Chapter Eight. I introduce them to be rebutted, replaced or improved, to illustrate what first steps might look like in formulating the form and content of the care information utility. Just as my GEHR ellipses diagram and subsequent original openEHR manifesto were in framing those embryonic ideas. To make it rhyme, I am calling this idea openCare!
The monad column is descriptive of values and principles on which we need unity if the scope of the co-created utility is to be coherent, clear and trusted. The dualism and dichotomy column represent complementary and contrasting choices and requirements that we must debate and seek to balance, staying true to the values adopted. The tripod and trifecta column groups perspectives and methods whereby coherence and stability of endeavour is achieved and sustained, within a dynamic equilibrium of a functioning citizen-centred care information utility and the related health care services that it supports. Again, these are not intended as clear-cut categorizations, but as a way to help describe, achieve unity in, and hold trust together in mission, method and community of endeavour, when seeking to implement the idea. They are not yet good enough and I have not discussed them widely. They are presented here in part as provocation, risking accusations of foolishness and woolly thinking (probably both still true) for others to improve, dismantle or replace with something different–hopefully drawing on practical experience of implementation. These are vertical lists, more than horizontal rows.
Table 9.1 is focused on terms characterizing information that is the currency of the care information utility.
|
Monad |
Dichotomy and Dualism |
Tripod and Trifecta |
|
care |
preventive and curative home based and institution based |
knowledge, phenotype, empathy |
|
confidentiality |
derogation and consent |
personal privacy, co-ownership, sharing of data |
|
equity |
ethics and law |
liability, accountability, responsibility |
|
identity |
autonomy and dependency |
family, kinship group, community |
|
coherence of meaning (also implying clarity and consistency) |
top-down and bottom-up |
education, research, practice |
|
common ground |
public and proprietary |
clinical, technical, organizational |
|
comprehensiveness |
self-directed and professionally determined |
interdisciplinary, multiprofessional, multiagency |
|
choice |
protocol and judgement |
risk, exposure, compliance |
|
continuity |
global and local |
time, place, person |
|
governance |
free enterprise and regulation |
public, private, community interest |
|
collaboration |
specialization and integration |
community, secondary, tertiary |
|
trust |
personal meaning and professional meaning |
head, hand, heart |
Table 9.1 Towards characterizing the information content of the Care Information Utility. Table created by David Ingram (2022), CC BY-NC.
Table 9.2 is focused on terms characterizing implementation that creates, develops and maintains the care information utility.
|
Monad |
Dichotomy and Dualism |
Tripod and Trifecta |
|
requirement |
global and local general and particular |
personal, professional, social commissioner, provider, user |
|
architecture |
centralized and distributed |
system, service, ecosystem |
|
design |
simplicity and expressiveness |
agility, adaptability, acceptability |
|
sustainability |
cost and benefit |
resource, method, team |
|
performance |
effectiveness and efficiency |
capability, capacity, opportunity |
|
resilience |
risk and safety |
knowledge, omnuscle, model |
|
affordability |
service and user |
current, medium term, long term |
|
standardization |
de jure and de facto |
global, national, local |
|
implementation |
public domain and proprietary |
rigour, engagement, trust |
Table 9.2 Towards characterizing the implementation challenges in creating and sustaining the Care Information Utility. Table created by David Ingram (2022), CC BY-NC.
Topping the first table is care; key to this, at the bottom, is trust–in what the information means and why it matters. Topping the second table is requirement; key to this, at the bottom, is implementation. We learn what to do and how to do it by doing it–iteratively and incrementally. The two tables share a connection through their concern for method–how to link information that supports care and trust with requirements and implementation of the associated information utility. Key to good care services and a trusted care information utility are guiding values and principles that frame the balance, continuity and governance of those services and the requirements and implementation of the coherent, citizen-centred care information utility that both reflects and supports them.
Care information utility is an idea and product of head, heart and hand. In such matters, actions and outcomes speak louder than words. Reinvention of health care services requires imaginative listening and response between the communities served and the professionals who co-create with them the environments that are needed and valued. Care information utility will grow on common ground created ‘somewhere’ that underpins the creation and sustaining of this reinvented reality. That is a David Goodhart ‘somewhere’, anchored in head, hand and heart.44 We cannot avoid carrying the load that is necessary for creating the ‘somewhere’ that we seek. Science has learned where and how to use information technology to keep a handle on its ‘somewhere’ signal and noise. It shares understanding of how to secure, standardize and trust its meaning. Society at large has not yet come to terms with care information in this way. Information created without meaning that is anchored somewhere and somehow can quickly degenerate into noise, anywhere, anyhow. Not very useful and not very trustworthy!
Utility is about values, principles and meanings. A good water supply means an adequate flow of clean water, delivered at a satisfactory temperature and pressure, and an acceptable price. A good electricity supply means a reliable and affordable source of electric power, safely and stably arriving at the point of use at a standard voltage and alternating current frequency, delivering adequate power for the task at hand, with electric current tripping off quickly if adverse events expose danger. A good heating utility means being fueled cleanly and safely, permeating the house, quickly switched on and off and from room to room. Coherent care information utility means support for safe, citizen-centred, effective, orderly, equitable and affordable health care. A picture of health is also a picture of care.
In the human body, the nervous system integrates and balances. If it goes wrong, balance goes wrong, too. Bodily balances are mostly not matters of conscious choice, although imbalances may of course arise that way. But information utility in health care is closely connected with choice and lack of choice in how health care is practised and made accessible. We must add choice to the issues of value, principle and meaning in play. Information in all these contexts cannot be metered by volume. But who is to judge information’s utility, in all these multi-faceted contexts?
Those best placed to judge meaning and value are those at the coalface of care, who experience it in their lives and work, pay the price and pay the bills. We need patients and those cared for to join in co-creating and sustaining information utility, side by side with the professionals, family and community carers and volunteers who serve them. Of course, we will need new tools and systems to enable and support them in this. Patient reported outcome measures is one good step along that pathway; they must be made accessible, consistent and mutually coherent. Many other parties will have more distant roles, making wider connections, and they, too, will have important parts to play in the creation and enactment of this new ecosystem–each qualified by the value flowing from what they can bring, make and do in the process of reinvention and reform of health care services.
In his 2020 Reith lectures, Carney connected the three global crises of money, climate and pandemic, and the learning from these, suggesting how this might impact in his new UN role. All three have common ground in imbalance of information and environment. They have escaped Pandora’s box and their rescue, according to Carney, requires new focus on values. Values are imbued by both nature and nurture. In the lectures, he left values on one side (perhaps inevitably and wisely), to focus on leadership of change. His prescription for change was top down, focused on engineering, politics and finance (new opportunity in innovation). In terms of method, he focused on measurement, risk management and returns–the latter meaning a focus on making socially desired interventions worthwhile and profitable to enact.
For a care information utility, values, principles, meanings and choice are all central and cannot be left on one side. Repeated prescription of things that have not worked, from the top down (a continuing prescription of the same interventions), should be paused, to allow greater space and resource for innovation in method, team and community, working from the ground up. This is where new trusted fulcrums of balance, continuity and governance of services can come from, to help cure ‘Shallow Medicine’, the term Topol used to characterize the uncaring predicament of medical practices, today.45 Carney’s risk management and returns are needed, and these can best be addressed within the wider governance of information utility. Vested interest conspires with status quo to minimize returns on innovation it does not want. It has little exposure to and awareness of poor quality of service and management of risk at the coalface of care. It has only indirect levers for influencing them, anyway. Money and management of infrastructure and workforce become their surrogates in pursuit of value.
My 1991 exploration of the topic of information explosion and its impact on clinical medicine, combined with confirmation by wise friends of the huge scale of the new challenge that I was about to engage with, confirmed my inclination to focus on practical implementation of digital health care records within the communities and environments that I had just started to join, in leading the European Union GEHR project.46 It was a new adventure of ideas: discovering, exploring and demonstrating the how, of how to achieve information utility for health care. Catch-22 has abounded when making such choices in the Information Age. We are at fault if we make and do, and at another kind of fault if we write and cite. A chimera of fox and hedgehog47 might be a fog or a ho(a)x! Theoretical fog or practical hoax–plenty of both of those around! Catch-22 has become catch 20-20. Above all, we need imagination around which to build a vision of the future that we wish for.
An Imagined Tomorrow
It always seems impossible until it is done.48
Costly burdens, waste, incompatibilities and obsolescence pervades the current health care IT legacy; intractable problems reflecting information systems not turning out as they were hoped and envisaged to. Five decades of effort have battled to alternately reinvent and contain this reality. As with climate change, it is a combined challenge of discovering new methods that can help make things clear and clean, and ways of working clearly and cleanly to implement them. How should we approach this challenge in pursuit of creating the care information utility? Not without a common ground of semantically rich platform architecture, I think. And not by adopting and imposing proprietary architecture, either. We must think from both global and local perspectives about how we choose, remembering at all times that we are envisioning something that is organic in nature, in the sense of ‘relating to, or derived from living organisms’ and being adaptable, evolving and humanly centred, to serve the different and changing needs of individual citizens for supportive health care services.
The case for reinvention and reform of health care services, and the practical realization of a citizen-centred information utility that supports it, aligns with a wider case for reform of public services. There is growing recognition that the assumptions that underlay implementation of the Beveridge vision of the 1940s, in the way that the National Health Service (NHS) was constituted, are no longer sustainable, on all sides–patients, professionals, providers and politicians. Failure of affordability, feasibility and effectiveness of this model of services, albeit multiply reorganized over time, has been laid bare in the anarchic, fragmenting and continuingly inequitable transition of health care services into and through the Information Age. Efforts to cope with ever-rising demand, set against limited resources and workforce, have focused on efficient management of demand and supply, aimed principally at dealing with and coping with acute episodes of need. These have consumed ever increasing resource and energy. In consequence, there has been insufficient attention paid to understanding the many and important causes underlying these needs and focusing priorities to support and promote personal and community capability and resilience in preventing and coping with illness and ill health and providing supportive care.
Local and community strengths that existed in Localton have not survived into Globalton and its ever-increasing and fragmented silos of needs, discontinuity of services and non-coherent data. People experience, feel and suffer from this reality. The Information Age opened multiple Pandora boxes of fragmentary ideas relating to questions that asked, ‘What is the matter with you?’ and drowned in non-coherent data conveying the fragmented answers. This has overwhelmed inclination or opportunity to pose and reflect on answers to the question ‘What matters to you?’ ‘Never mind’ is not a good answer when hearing about what matters! We need an information utility to guide and support services and actions that get closer to the heart of the underlying causes implicit in the answers we hear and prevent as many as we can of them from happening. We may then gain greater capability to act promptly, effectively and humanely in matters requiring urgent care, rather than become increasingly overburdened in coping with their unmitigated consequences. The information utility must therefore be very much citizen-centred and focused on preventing, anticipating, coping and caring. To be citizen-centred is to be rooted in local context and contingency, not in an imagined helicopter view.
Thinking and exploring along these lines, experiments in local UK Government (Wigan and Barking) have pooled budgets of fragmented services and explored unified service models, under common ownership and governance of solutions that are tried. They have saved money and improved citizens’ experience of their services. Bob Jones’s Continuing Care at Home (ConCaH) story of thirty years ago and the family receiving twenty-seven unconnected visits from ‘support’ services in one week (as described in the section on continuity of care in Chapter Seven), is paralleled in similar stories, today. Yesterday, I heard described a situation of twenty uncoordinated visits and visitors similarly arriving at the door of an elderly patient discharged from hospital, to provide care, but unaware of and unconnected with the network of family and neighbours already there and primed to support.49 We cannot continue to have one episode of discharge from hospital ramifying into and through the Cloud data stores of twenty non-coherent care records.
Maybe we should start by taking note again of a comment attributed to F. Scott Fitzgerald (1896–1940) in ‘The Crack-Up’, published in the New Yorker Magazine (1936), that ‘The test of a first-rate intelligence is the ability to hold two opposed ideas in the mind at the same time, and still retain the ability to function’. We should not funnel all our efforts along single paths through the wood or devote all energy to prophecy, debate and conflict about their merits and demerits. We should raise our sights to the level of purpose, goal and method–to making and doing things on incremental scales and learning as we go. We really should stop inventing large-scale, nationally ‘imagineered’ initiatives, that swing all concerned dizzily from one scramble for resources to another, and repeatedly disrupt all in their path. We should focus more on imagining the coherent common ground required for any approach to succeed, and collaborate as engineers of all disciplines and callings, to create, evolve and sustain it.
The openCare endeavour will be of moonshot dimensions and duration and will exercise the best of the best. But approached collaboratively, across countries and institutions, it can be made tractable and affordable, if tackled as a well-articulated vision, and in the right spirit, better-expressed and contextualized than I have managed to frame it here. Somewhere, somehow, in whatever increments, we need to give it a go. I believe it will be, for many key people, a career-defining goal, just as openEHR was mine. It can only succeed when locally connected, implemented and governed within a coherent global context. History and experience suggest that it cannot be achieved in the world of governments or industries, and neither can it happen without them. It requires community-led enterprise and continuity of method, throughout: rigorous design and associated tooling shared in the Creative Commons; engagement with health care professionals and citizens at the coalface of care; inclusive participation of public, private and voluntary sector; connection within international community that shares common cause. These are all necessary in setting the scope of an approach to implementation of a care information utility. But they are not sufficient for gaining traction in how it is achieved. For that we need a shared vision of what we are aiming for.
So here goes with one such organic envisioning (Figure 9.4). Everything must start somewhere! Again, this is not intended as being a technical specification or health care reality. It is a purely imaginary picture inspired by Maurits Escher’s (1898–1972) Circle Limit III woodcut.50 The diagram is an Aunt Sally, to focus debate and be improved on, just as my GEHR ellipses and openEHR manifesto were.
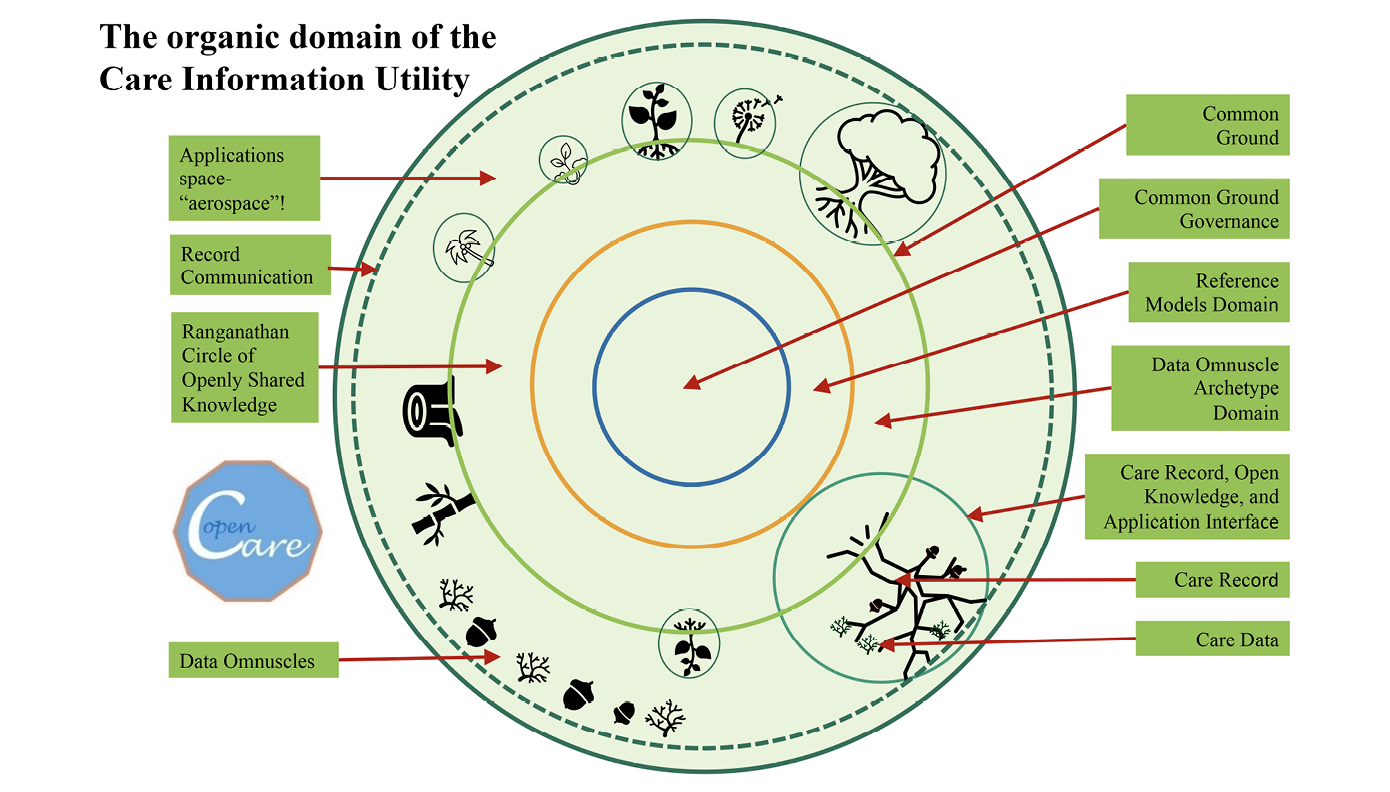
Fig. 9.4 An imagined organic ecosystem of the Care Information Utility, inspired by Escher’s Circle Limit III woodcut and the journal Nature’s characterization of Suzanne Simard’s vision of forest ecology as a ‘Wood Wide Web’. Image created by David Ingram (2022), CC BY-NC.
In Escher’s organically inspired woodcut, the infinite and fractal patterns at the periphery of the circle grow into central, swimming, fish-like forms and structures, and dissolve back outwards again, into an infinite variety of manifestations. For me this mirrors the fractal nature of the health care knowledge and data domain, thus characterized by my clinical colleague, Tony Shannon, who pioneered theEtherCIS open-source openEHR platform initiative, as described in Chapter Eight and a Half. My picture here is inspired by the forest-like information ecosystem described in Chapter Eight. It depicts this ecosystem, above and below ground, with zones labelled as components of information utility fitting in with this metaphor: data and connecting data formalisms; circle of knowledge and connecting knowledge formalisms; care records and connected record formalisms. The common ground is where coherence of clinical data models, reference models of the patterns of data drawn on, and where the governance that aligns these within systems and services, locally and globally, is anchored and resides.
The records and data are shown with diverse tree and plant like omnuscular shapes and forms, omnuscle being the term I invented in Chapter Three, to characterize clinical data elements and compositions. They are rooted, communicate and propagate within the forest, above and below ground, and are transferred through the air above ground. The green circle is ground level and encircles the common ground around which the utility revolves and evolves, in an imagined (fanciful) applications EHRospace! The governance of this citizen-centred utility operates from the centre of this common ground.
The diversity of message formats in the EHRospace is not the issue (do not shoot the messenger!). What matters is the coherence of the semantics and contingency of the data collected, according to the formalisms of data and knowledge residing within this common ground, that conveys (or fails to convey) the coherence of their meaning for the individual subject (person) of care. We need global design combined with local customization and governance of a shared common ground of information systems to underpin an information utility fit for purpose in supporting the balance, continuity and governance of health care services.
The transition to an ‘organic perspective’ (organic here carrying the same sense as Whitehead’s application of the term to his process philosophy, as mentioned in Chapter Two and further elaborated on in Chapter Eight) of care information utility, is inherently uncertain and will continue to be so. But the transition is nonetheless very necessary for conveying meaning in the highly contingent world of health care. It will take us into a new world of requirements and methods for formulating, accessing and managing information. Diverse, ill-formed and loosely connected information systems have amplified difficulty and uncertainty in coping, loosely, with these sorts of requirements. But the progress captured along the timeline traversed in this book has brought considerably greater clarity and certainty into ways of tackling these challenges in the future. We are halfway there in devising means to approach the clarification and cleanup required. There remains the considerable problem, though, of how, iteratively and incrementally, to supplant the burdensome legacy of creaking and maladapted software and systems from the past fifty years, that is still relied on to support increasingly costly and overburdened services. I am not thinking here of hospital systems or vaccination systems, general practice systems or any clinical management systems. I am thinking of the individual citizen and what involves, and matters to, them, in all these multiple contexts, as well as their common ground and grounding.
Putting the data together, and putting the records and services drawing on the data together, are two different concerns–both important and mutually dependent, but different. Modelling and reasoning with knowledge, modelling information in its roles in support of actions, and modelling related data through their evolving and declining life cycles, are different but closely related domains (knowledge model, information model and data model, as discussed in Chapter Five), each requiring different methods and governance. The history of these domains has not easily coped with and come to terms with these wide-ranging connections, buffeted by ever-changing technology and requirements for survival in service, professional, academic and commercial contexts. It has dealt with them in isolation, writing and pontificating copiously, but comparatively less emphasis has been placed on implementing, learning and connecting at scale.
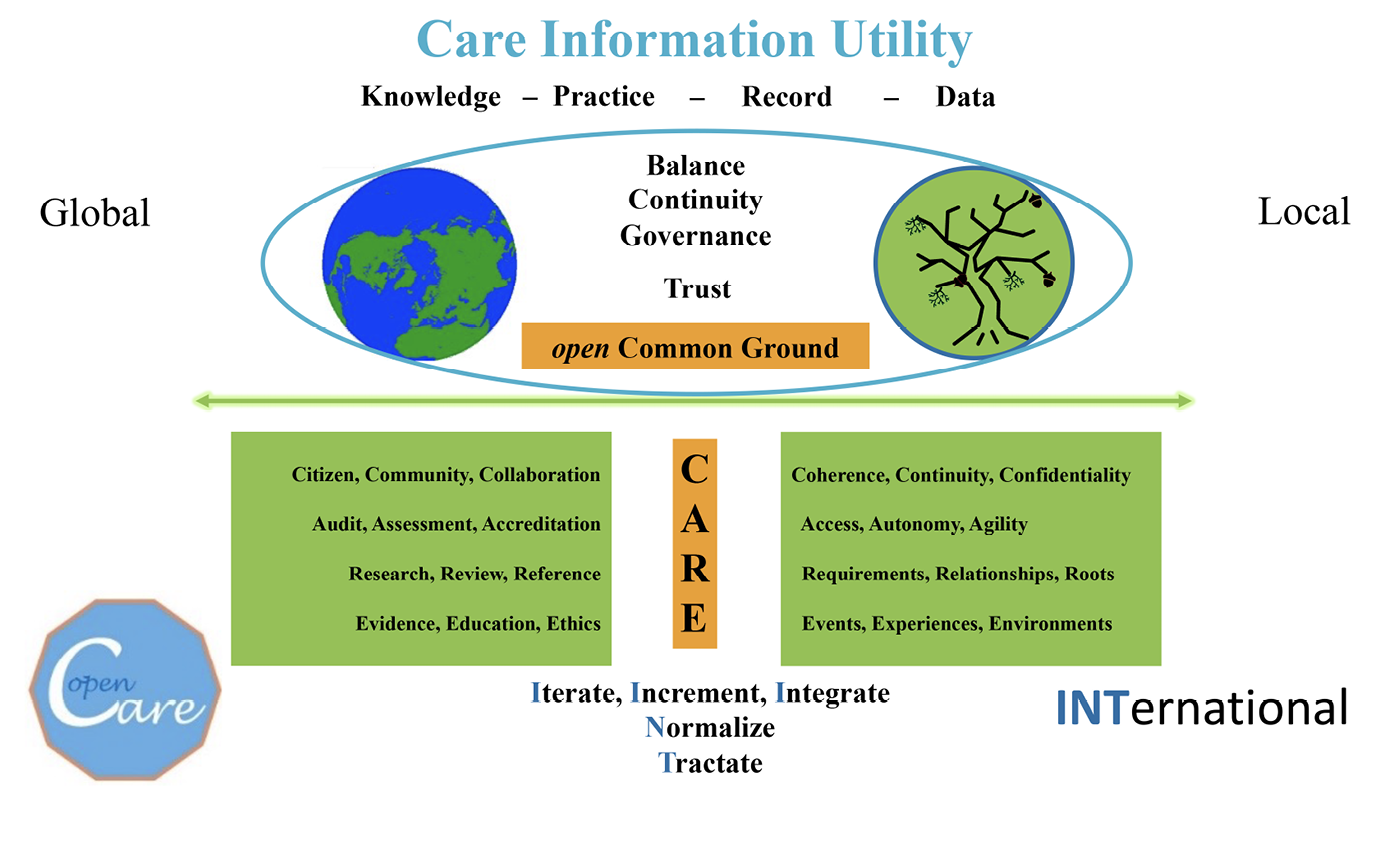
Fig. 9.5 Creating coherent common ground on which to base the openCare Care Information Utility. Image created by David Ingram (2022), CC BY-NC.
Mervyn King characterized our era as one of radical uncertainty. This is notably true of health care. I have attempted to express in one diagram (Figure 9.5), again rather contrived and ethereal at this stage, what seem today to be suitable inuksuk concerns–defining and guiding landmarks–signalling a path towards greater certainty in health care, with their initial letters spelling out CARE, expressing the pervasive scope of a care information utility.
Throughout, a balance of global and local perspective and governance is depicted, with concerns of knowledge merging into practice on the left, and of data accumulating and aggregating within record on the right. Balance, continuity and governance characterize and anchor the trusted common ground between them. Coherent common ground is where greater clarity and certainty must obtain if co-evolving knowledge and record are to cohere within an overarching and trusted care information utility, supporting a caring service.
And, in addition, the words with initial letters INT spell out how its implementation should be approached. It is a play on both letters and words, intended to stimulate controversy as much as anything. I hope it gels well enough in that regard. Taken together CARE and INT conveniently spell CERTAIN! The elements shown depict the broad scope that this greater certainty must embody. How it can now be achieved, joining values, principles, methods, implementation, people, services and environments, is the challenge we face. It is a challenge we have to meet but we can only do this iteratively and incrementally. There is no helicopter-viewed solution that short circuits that path.
Citizen, Community, Collaboration: Coherence, Continuity, Confidentiality
The care information utility is a bridge between the autonomous citizen, in the context of their local community, and cooperation among the professions and services of health care, and with concern for coherence, continuity and confidentiality of data and record. It has two modes–one facing towards the professional teams and the other towards the citizens they serve. Its central rationale is the communication of meaning. It democratizes knowledge, enables quality and continuity of professional practice, and empowers and supports citizen and local community autonomy. It is both a global and local integrator, under both global and local governance. It must be free at the point of use.
Audit, Assessment, Accreditation: Access, Autonomy, Agility
The data and records of the care information utility focus on providing agile configuration of its content and access for autonomous citizen and professional users. It anchors wider purposes of audit, assessment and accreditation, for personal use, and community and professional governance.
Research, Review, Reference: Requirements, Relationships, Roots
The care information utility is a reference library and knowledge base–joining research and review of the professions and what matters to them, with the requirements and interests of citizens and what matters to them. It is a resource in support of citizen science which will greatly enhance the scope and validity of achievable epidemiology and health care services research. It will support and integrate research alongside education, training and practice. It formalizes record-keeping and its connecting relationships with and rootedness in knowledge and methods of data capture, analysis, reasoning, explanation, decision and action.
Evidence, Education, Ethics: Events, Experiences, Environments
The care information utility is a bridge between data and record that captures the events, experiences and environments of personal health care, with aggregation and accumulation of evidence within an ethical environment of health care systems and services, providing information resources that underpin and enable formal education and lifelong learning.
Iterate, Increment, Integrate
The care information utility is an integrator–it bridges from the iterative integration of data and record to the incremental advance and integrity of knowledge sources, alongside personal and professional, accountable action. Figure 9.6, along with Figure 7.8, illustrates the breadth of integration of information involved in dual support of knowledge and practice.
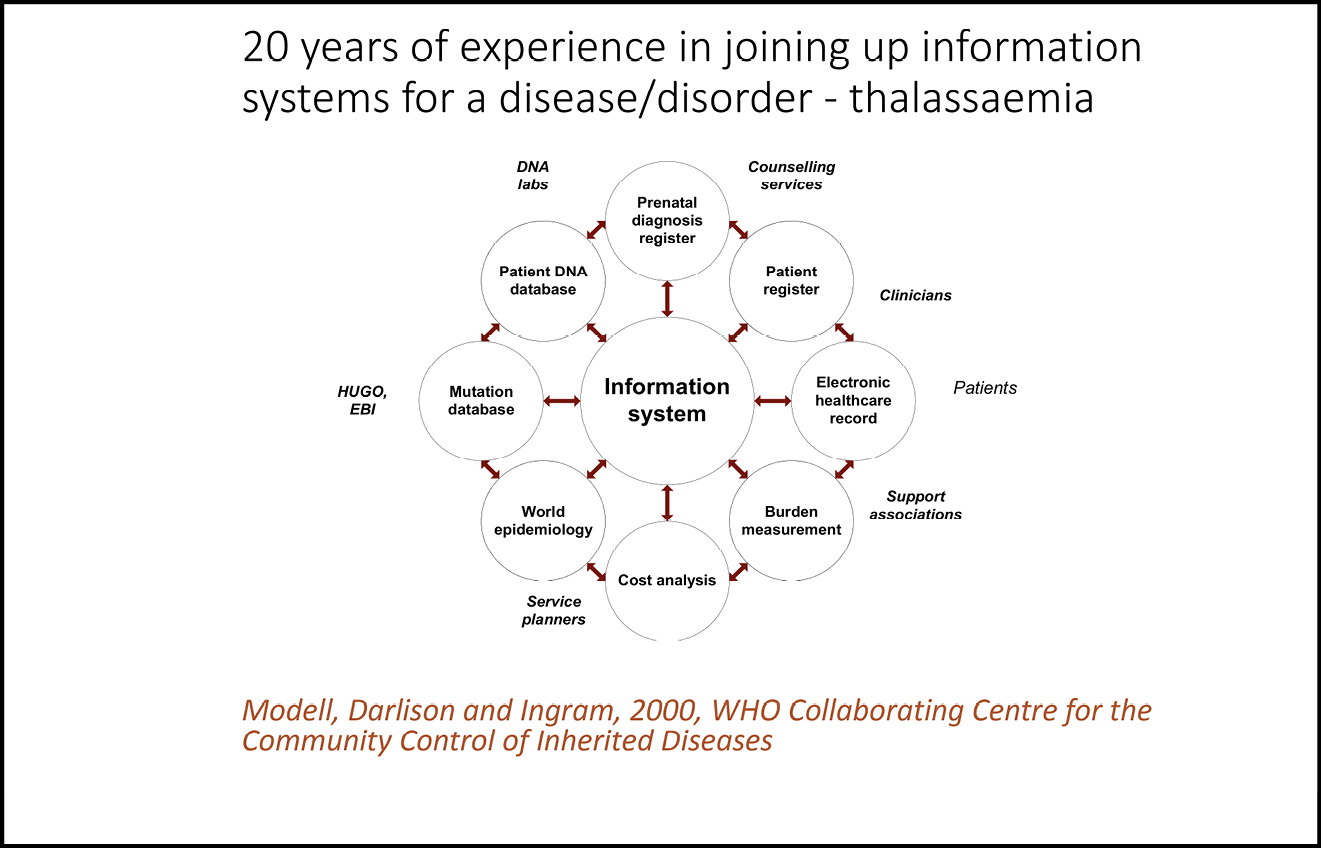
Fig. 9.6 The integration of information sources drawn on in formulating the APoGI (Accessible Publication of Genetic Information) utility developed at CHIME in UCL for patients affected by thalassaemia.51 Image created by Bernadette Modell, Matthew Darlison and David Ingram (2000), CC BY-NC.

Normalize
The care information utility is a bridge between domains of standardization–norms of health care practice and normalization of data, record and knowledge-based systems used in the delivery of services. Common ground of standardization underpins ways of working and the architecture, design, operation and governance of information systems.
Trust and Traction
Trust is central to cooperation and collaboration; traction is central to effective action. Data and record must have traction. Traction in working incrementally at appropriate level and sustainable scale. The growth and preservation of trust involves head, hand and heart–expressed in education, experience, commitment, action and belief. It grows along all these axes through actions that speak louder than words. Robert Axelrod’s insights, as expressed in his book The Evolution of Cooperation, on the building of trust, are central to the values and mission of the information utility, expressed in its methods, practice and governance.52
Some of this daunting range of topics will be more amenable to consensus and others more prone to contention. The diagram serves to complement Topol’s declaration that reinvention of health care, from ‘Shallow’ to ‘Deep’, must be focused on reinvention and rediscovery of the capacity to care–period, he says, emphatically, to which I would add open care, period! The utility must be approached as a global public good, much as openEHR and OpenEyes have been and are increasingly seen.
These letters (CARE and INT) also conveniently line up in expression of openCare as an international mission or as openCare International! As with openEHR International, the world will tend either to love or hate openCare International. Zobaczymy!
Incremental Goals–Promoting Trusted Balance, Continuity and Governance of Care
All knowledge of reality starts from experience and ends in it.53
A journey of a thousand li [miles] begins under your feet.54
The accumulation of knowledge is intimately connected with the capture of experience. It is a difficult, long and winding road to the creation of a viable citizen-centred care information utility, but we must not be afraid of and avoid travelling it, thereby making things harder. We should approach it purposefully, a step at a time, by framing of specific goals on which we set our sights, towards which we then navigate. I suggest some candidates later in the chapter.
The amount of data routinely collected in health and social care settings has increased massively in the Information Age, whether strictly exponentially, or not. We know that data capture costs time and money and adds burden to health care services, with more data not necessarily correlating with or guaranteeing better outcomes, and overload of information risking poor decision making. We know that fear of legal blame may lead to defensive, repetitive and over-investigatory professional practice, whether for reasons of caution or financial gain. The resulting segregated silos of data and record lead to poor continuity of care. These multiple factors can easily combine towards redundantly expensive, time consuming, inconvenient, inefficient, ineffective and potentially harmful practice.
We know that citizens have access to knowledge as never before and this changes the balance of citizen and professional relationships, where patients as individuals, groups of patients with similar conditions, and local and national charitable and voluntary sector organizations engage more knowledgeably in matters of practice, support and advocacy. We know that concern for protection of the confidentiality of personal data has increasingly been expressed in law that places a high burden of responsibility for compliant practice with people and systems, responsible as custodians and handlers of these data.
We know that obsolete software becomes increasingly difficult, and then impossible to maintain and use. And that the cost and disruption caused in switching between systems places a brake on change required to keep pace with increasing medical knowledge and changing nature and organization of services. We know that standardization is a precondition of coherent information systems in support of continuity of care and the communication of content, context and meaning of care records. And we know that these are complex and contested matters and interests, set within the context of competitive markets for products.
In all these aspects, there is a balance of individual, community, professional, commercial and wider public interest. A balance of rights and responsibilities as expressed in law. A balance of the art of the possible in framing implementation and operation. A balance of fairness in access to health care services and support. These balances are essentially those that I set out in Chapter Eight, when framing the scope of a care information utility.
In seeking to cope with all this complexity, we need always to remember that there are only individual citizens, patients and professionals who are being cared for and caring. They are not fragmented human instances in these separate and fragmented domains of service activity: a resident of a care home; a GP; a community nurse; an occupational therapist; a social benefits claimant; a cardiology or cancer patient being treated by organizations based in a nearby or faraway city, that deliver their services through a network of district hospital outreach clinics; and so on. The ways in which the identities of people and their human interests become fragmented instances within databases, to serve the needs of the fragmented information systems operating in these separated and differently governed and regulated domains, impact us all–those treating and caring, those they serve and everyone who picks up the tab and pays the price.
The records attached to these fragmented identities can easily become noisily, inconveniently, inefficiently, expensively, ineffectively and unsafely inconsistent and inaccurate. Conflation and discontinuity of values, principles, purposes, goals, methods and outcomes can become deeply engrained within information systems, placing aggravated strain on the tripods of implementation that I have described above, whereby the struggle to maintain stability plays out. Tripods fall over, squares are better, but a circular foundation is the most stable. The common ground is a circle of knowledge, data and information utility, with services encircling the citizen, rather than citizens encircling each service.
There is an expanding and evolving landscape of information, adding to this fragmentation of identity: genomics data; the internet of things with devices everywhere monitoring, reporting and guiding management of chronic disease; the alerts and advice of AI based on Big Data. Such machine-based representations and their data explosions can come to disorientate and condition human sense and sensibility.
I am exaggerating, of course, but things do not have to, and should not, go this way. We must signal, steer and nudge in a different direction, where we do not just pay lip services to patient-centredness and then align all the data and records around multiple different centres of health care services, devices, organizations and IT systems that splinter the individual subject into multiple proprietary and secret representations. There are, and should remain, markets, and they will do their work in incentivizing innovation and investment for change, and there must be associated recognition and reward. But we should remember that we cannot do science without sharing systems of measurement and models of reality. We may use different ones–standardization does not necessarily imply uniformity. But it does imply openness, sharing and trusted governance. Only in this way can we learn and act to do things well, and improve and replace our systems safely, without unnecessary encumbrance of legacy, over time. These considerations have not arisen uniquely in the Information Age, but it has amplified and highlighted their impact. We need common ground of language, method, community, governance and trust, to hold our endeavours together–otherwise we will continue building Escher’s unstable Tower of Babel–a biblical construction seeking to reach towards God, but arrested by God, who created confusion of language such that the builders were unable to understand one another!55
In the early information era, spending on systems was perhaps eighty percent on hardware and machine environment and twenty percent on software. This is just an 80-20 guess, the precise number would be variable in place, time and context, anyway. The hardware was the utility. Over decades, this balance inverted, and software became the eighty percent utility and hardware a twenty percent commodity. Now software, too, along with hardware, is increasingly a commodity, and the costs incurred are moving up another level, into the user domain, building towards information as a utility–with adaptation and replacement of health care services, accordingly. It is a semantically tuned utility, capturing, reflecting and integrating with social and professional goals of health care, and moving beyond the machine and software constraints that have dominated and beset them for fifty years.
We could never envisage a project to realize this new stage of evolution by approaching the care information utility as a software stack, any more than we could envisage ideas of life and consciousness constructed from the biophysics of cell membranes and the magnetic resonance imaging (MRI) brain scans of neuroscience. These insights help significantly to illuminate and systematize our knowledge, but they do not in themselves integrate. Understanding of life and consciousness exists at a higher level of information and meaning, and thus it is with information utility for health care. Care information utility embodies an ensemble of values, principles, meanings and choices, along with purposes, goals, methods and actions, and the governance of this enterprise must reside where those meanings play out in society.
But we do, at the same time, need to understand and control the technical, professional and organizational architecture of the utility, and adopt policies that can start to be implemented, incrementally and rapidly, at scale. We need to pick pieces that can be configured and connected, and then, as with a jigsaw puzzle, assembled, piece by piece and section by section, into the evolving structure of the utility. We need purposes, goals and methods that persist, throughout. We need team and environment. We need resources and governance. We need commitment, ownership and trust.
A common ground of method, owned and freely accessible in the Commons, will enable and empower the valuable resource of students, volunteers, companies, countries, charities and funding bodies, to participate in and, importantly, feel valued as a part of the endeavour. The governance of infrastructure and method should be global, clear and concise, as small as possible, and characterized by a light touch. The harder the challenge, the simpler its framing needs to be. The governance on the ground at the coalface should be locally contextualized and owned and built with the local community and within the Creative Commons–extending upwards in terms of sharing of method and outwards in alliances and sharing of endeavour.
All should have interface and connection with the organic information utility, which should be allowed to grow, as trees planted and nurtured, not as a grand design imposed and erected far off. It should exist and scale through the building and sustaining of alliances, because it works for them, not because someone says it should work. It should supplement, enrich and enable health care of today, under its own momentum, consuming resource commensurately as it proves itself in practice and scales. This is about design, organizational development and campaign–about the people who are motivated and can make it happen, because it creates a better world for them in what they need and wish to achieve. Where commercial enterprise ticks these boxes, it can and should take root within an information utility, as well, just as a voluntary agency, charity, public enterprise or other community interest can and should do so. There are huge resources available to be drawn on and the utility can join up and spread nationally and internationally.
The care information utility is an evolving ecosystem:
- Its methods are a shared common ground;
- Its values and principles are expressed in the monads;
- Its balance reflects the dualisms and dichotomies;
- Its continuity rests on the tripods;
- Its governance works to articulate and promote community interest and engender safety and trust.
Returning to the perhaps overly poetic forest symbolism of Chapter Eight, it is an organic network and should be seeded as a new forest on common land–alongside legacy forest. Like the Heartwood Forest we often walk through, governed by the Woodland Trust, bringing together the human and natural world, as users as well as professionals and volunteers, onto new common ground and forging new connections, from ancient woodland to newly planted trees. The ground occupied should be the common ground of all health care communities, where they will plant new seeds that can germinate, grow, connect and communicate more straightforwardly, on new ground. These will connect with, and over time supplant or enable, the reinvention of the legacy of siloed data and record. Some citizens will choose to engage under the canopy of the information utility, and some not, with consequences that flow.
Some areas ripe for such incremental reforestation goals might be:
- Chronic conditions–monitoring, treatment and progression;
- Patient Reported Outcome Measures (PROMS) and vital signs;
- Component data descriptive of patient state–allergies, for example;
- Dashboards of community services and specialisms, summarizing activity, health status and quality of services;
- Continuity and logistics of care–shared care records;
- Platforms that integrate cognate services at all levels–for example, continuity of eye care, from High Street opticians providing spectacles to tertiary treatment of eye injury and disease;
- Perinatal care;
- End of life wishes;
- Hospital at home–community care, teleconference, telemetry of vital signs;
- Keeping fit and well–approach, interest and opportunity;
- Medicines management;
- Infection control;
- Screening and vaccination.
Implementation Two–Endeavour–Where, Who and When
We now come on to the where, who and when questions. Through whom–in terms of people, teams and leadership–and in what kinds of environment should the pursuit of purposes and goals of the care information utility be taken forward? When and over what time? These are big asks in the destabilized world of health care that we are living and learning through. Each fragmented component of the health care system has an interest that it defends–none can make progress in isolation, and no one can own and lead the whole endeavour. Successful formulation of such a complex endeavour is the second implementation challenge of the care information utility. Rival stakeholders doggedly lock claws on battlefields and contrive something akin to the lobster quadrille of Charles Dodgson (1832–98) (a mathematician and author, better known as Lewis Carroll, whose Snark hunting headlined the previous section), emanating downstream in a computer-software-like deadly embrace!
Admittedly these are huge challenges, but scale of challenge does not always necessitate, or benefit from, scale of endeavour and enterprise–it may be a Fred Brooks mythical man month challenge,56 requiring the seeding, nurturing and growth of new ideas, and their exploration in implemented prototypes, by new people in new environments, where scale attempted too early may prove counterproductive. It may require Suzanne Simard’s level of dogged and persistent individual courage and insight, whereby endeavours like hers have prevailed in resetting understanding of the ecosystem of the forest and its health.57
Endeavour is anthropology writ large–Tett, in her book Anthro-Vision, describes how she sees anthropology contributing to the understanding of human endeavour.58 Without delving too deeply into belief and philosophy, a human endeavour might be described as a creative circle that connects what, why and how with who, when and where, aligning people and environment with adventure of ideas. As Whitehead said, adventure of ideas lays the foundations of programme for reform. Creative endeavour is an iteratively and incrementally connected set of solutions to problems encountered. Progress can involve a good deal of costly endeavour, failure and lost time. Seventy years and counting in health informatics and care information utility!
Record of endeavour, like record of care, starts with questions: about who and what. It captures facts about people and what happened. These questions broaden: Who participated where, when, how and why? Where, when, how and why also pertain to the factual record–about environment and time, and method and purpose. Questions about people, method, environment and time capture issues of capacity, capability, appropriateness and timeliness. Creation of care information utility needs capable people, in conducive environments, with necessary connections and resources, and suitable governance, doing appropriate things, in a good way, at the right time. A challenge, at which it would be easy to throw up one’s hands!
Two inukbooks have provided a useful guide and perspective about the human dimensions of doing better things in better ways, among communities of sometimes uncooperative and disagreeing participants (especially the clever ones, possessed of the conviction that they know best–which they sometimes do, of course, but not always!). These are The Evolution of Cooperation by Robert Axelrod, in its analogies with games theory, and Getting to Yes, by Roger Fisher (1922–2012) and William Ury, with their insights on the principles of negotiation.59
Co-creation and use of the care information utility are inseparable, just as health and care are inseparable. Balance, continuity and governance of the utility created, are essential. So, too, are its community and working environment of implementers and users. The interaction of different people and perspectives, assembled over time and in close propinquity, was central to the utilitarian philosopher Jeremy Bentham’s (1748–1832) felicific calculus–a calculus of happiness. Human community and environment are the essence of that happiness and sense of wellness. The quality of community and environment in which care information utility is created and sustained will reflect in the values and meanings attached to it. It will be a co-creation by developers and users–there is no waterfall from creation into use. Implementation of the utility involves the joining of its people, environment and use, and is an intrinsically organic and local concern, where it is used. Coherent purpose, goal and method adopted for the creation of the utility will underpin its continuity; these aspects are intrinsically global in nature. A fragmented utility that lacks global coherence will not promote balance and continuity in the local purposes it serves. Global and local governance must maintain balance of global and local perspectives.
Such ‘we’ not ‘I’ thinking is on the upswing in our grandchildren’s generation. It was equally partitioned over time in my parents’ lives–first on the upswing and then on the downswing. The Information Age has been created on the downswing, and it shows. The Information Society must now be created on a tide of upswing. Putnam, the author of The Upswing, as described above, predicted that society today is at a nadir, poised for a reversal from downswing into upswing. Let us hope the nadir is not too noisy!
Diverse and overlapping mechanisms make for resilient and fault-tolerant bodily health. They are likewise intrinsic to strength of endeavour. Health care needs are diverse, as are the services that support them. Diversity is not the same as fragmentation–diversity encompasses while fragmentation breaks apart. We need an information utility that encompasses the whole of health care and enables inclusive and holistic, rather than fragmented, endeavour. Policy must reflect diversity, but a fragmented diversity of policies directed towards a common goal is a recipe for inconsistency, waste and ineffectiveness. The nature of wicked problems is that they lend themselves to this sort of policy fragmentation–everyone and no one owns them, every approach and none is applicable, and political estimation tends to trump policy implementation at every turn. And when we computerize, we are dealing with a technology that does not naturally embody diversity and stokes fragmentation–we are best not to code a diversity of sampling and analysis algorithms to collect a common dataset, such as the NHS had to cope with when instigating central reporting of critical incidents, as discussed in Chapter Seven. Where such inconsistency prevails, official statistics exhibit computer generated noise and bias as a result. But it does not need to be that way.
Environment
Good environment (to repeat Richard Wollheim, yet again!) is a necessity. An organic information utility can only grow from the ground–it cannot descend from the information forest canopy. Creating the environments in which it grows is about bringing together the complementary teams and expertise required, on the ground, and supporting them and meeting their needs, too, over time. Environments where iterative and incremental adaptation and change can be harmoniously embodied as the utility permeates and disseminates, organically, in its development and growth. Environments where complementary teams, leadership and governance seek to cohere, whereby circles of users, communities, professions, organizations, industries, regions and countries, can draw together and cohere in pursuit of shared vision and common goals. Environments that are at one within the information utility they create, sustain and participate in, anchored on the common ground that they share.
We participate in and experience multiple environments in our lives and endeavours, catering to different interests and responding to different needs. We make of them what we wish to, while we can or must. They shape us and we shape them. Environment, teamwork and leadership of innovative endeavours are complex interactions. First impressions count–one learns a lot about an environment when first setting foot inside: about leaders when first meeting them; about team and mission when first sitting with them.
A Songline of Environments
In this section, I describe and compare a diversity of creative environments and complementary endeavours that I have experienced first-hand. I start in care, travel through education, medicine and health care, in public, private, charitable, commercial and community interest environments, and finish back in industry and naval shipyards. These environments, and the people I met and worked with there, interconnected and cross-fertilized along my songline. Some names and connections crop up in several places, illustrating those interconnections and what flowed from them.
Care
In her twenties, my mother worked with Francesca Wilson (1888–1981) and Edith Pye (1876–1965) to create a safe environment in Barcelona for refugees displaced by the Spanish Civil War. Fred Sanger (1918–2013) and my dad, and the many others at the Spiceland Training Centre, were creating a new environment, seeking to imagine and construct it in everyday community life. I lived for the first twelve years of my life in the rural environment of a large residential children’s home run by my parents, caring for twenty-five English children, separated from their broken families, and helping them develop and grow. It was a good environment, founded quite simply, in a lovely, very large house, twenty acres of fields, woods and streams, children playing, eating, sleeping, fighting, climbing and falling from, trees, coping with personal trauma and distress, scarcely ever visited by family they had lost. It was a safe and orderly place, and it was a caring environment–that was what made and helped knit back together the pieces of each fragmented picture in each person’s mind. It did a lot to reintegrate the fragmented wartime lives experienced by my parents. A picture of health is also a picture of care. Information utility is a picture that connects health and care.
Education
Some environments are transformative, some are short-lived and others last. Some are revolutionary and others stabilizing. For me, later years at school and in university days were transformative. I advanced further and did not much look back. Life was busy and fun. It opened outwards–a shy boy isolated in a children’s home that was organized around the needs of community more than family, found liberation in study and skills in maths that led to a physics scholarship at Magdalen College, University of Oxford. The experience and learning that came from coping within the children’s home community bore fruit and helped to convey this boy into an industrial scholarship with the Vickers Group of companies. Sponsorship from a family friend funded him on an exchange visit to the USA, from New York and Washington to Louisville, Kentucky, and friendships made there lasted through many decades, until his family hosts died. These were totally new and complementary environments and experiences, and, taken together, they added up and I was lucky.
Medicine and Health Care
My songline has taken me through a diversely connected range of health care working environments, from neonatal to adult intensive care, in primary, secondary and tertiary care institutions, in diverse clinical specialisms–cancer, cardiology, ophthalmology, nephrology, mental health care and care of older people–and in imaging and other hospital-based medical physics departments. I have worked in and visited them in the UK and overseas, comparing and contrasting. Connecting from one to another of these has been a formative experience for how I think of the professional context of the care information utility.
After leaving industry and moving to University College Hospital (UCH) in 1969, I experienced the everyday working environments of academic medicine and health care service departments, and hospital life, for the first time. Over the following years, I experienced them as an outsider, inside, engaged in the academic, professional and practical worlds of medical physics and medicine. To an outsider, the increasing fragmentation of health care, as it headed into the Information Age, was already in expanding view. Perhaps this was not so visible from the pedestals of the medical profession, betimes intrigued and threatened by the new technologies and tools transforming clinical measurement and intervention of the Information Age, but also facing increasing challenge about its own discipline and professionalism. This reflected in local institutional and national politics of rivalry, complexity and confusion, about the interplay of different levels and specialisms of health care. It was a prelude of transition from trusted and delegated professionalism of services to centrally controlled management of the organization and delivery of health care. It was also a tough era. In how it was received and used, the infant computer both enhanced and exacerbated this scene–on the one hand, it brought an increasingly magnificent new quality of medical imaging; on the other hand, it brought increasingly costly, time-consuming contention over largely unwelcome, often dysfunctional, computerization of hospital workflows and management.
By the good fortune of sponsorship by John Dickinson (1927–2015), who saw potential in my PhD programme as an innovative addition to his predominantly educational mission as the new chief of medicine at St Bartholomew’s Hospital (Bart’s), in 1976 I landed in the middle of an academic and professional clinical environment. This environment was a department situated immediately above the main medical and surgical wards of the hospital. I was, once again, an outsider, inside, viewed with understandable suspicion by the College authorities, the College physics department and some of the senior clinicians! I worked alongside the clinicians, but not with them, as they worked long hours. I got to know and helped some of the junior doctors cope with the demands of research and career progression. There were other non-clinicians there, integral to the department’s academic mission. Among them was David Perrett, a creative and practical biochemist, pioneering high-pressure liquid chromatography, who became a close colleague. We were a bit like a servant community, below stairs in a country house, with the clinicians as family aristocracy! They were sometimes lonely years. David’s practical grounding and commitment established him as a key player in a wide range of clinical research. He was on his similar, quite isolated, journey in the Department, that turned out very well for him, too, in his field.
I was equipped for such a challenging environment. It was not a million miles from how life in childhood had felt: viewed with suspicion by some in the children’s home, because of my otherness, and perhaps resentful of my privileged parenthood; and viewed with suspicion by some primary school classmates, perhaps a bit envious of my academic success. I was used to being an outsider and in so far as there are outsider skills, I had them, combined now with a sense of their utility in times of change.
I discovered new opportunities as I helped the young doctors and continued my mathematical modelling work with John. With the combination of interest, skill and experience I brought, I quickly found my way into new national programmes of educational computing, and later into creating innovative educational resources for charitable foundations, such as the Marie Curie Foundation for cancer care, and the Wellcome Trust for tropical medicine. This was the time that Wellcome became hugely endowed with investment funds and transitioned into its rapidly growing role as a major international funder of biomedical research. Each of these environments brought new experiences of health care community and environment. In each, I interacted with multiprofessional teams and their leadership–we were engaged on high-profile projects. Established medical journals showed little interest in educational innovation, being focused on new frontiers of medical science.
I was sought out as supervisor of medical physics PhD students, the first being Bill Flatman, who went on to a successful career in health care informatics. Through Paul Turner (1933–94) and Jim Malpas (1931–2019), eminent academic colleagues leading the Departments of Clinical Pharmacology and Oncology, respectively, who got to know me, I was asked to take on statistical peer review for medical journals. With my mathematical background and having taken on some statistics teaching in the medical student curriculum, this was a world I had come to know quite well. From there, I was made a fellow of the Fellowship of Postgraduate Medicine and member of the editorial board of its journal, connecting me with the world of publishers. Knowing the world of finance from my industry days, I was made Treasurer, and set about reorganizing and re-tendering the management of its investment portfolio, connecting me with the world of investment managers. There, I recall meeting the young Kate Bingham, years later the leader of the much-feted national Covid-19 vaccine task force. The Fellowship drew together a very interesting group of people from right across medicine. And then I was made a professor and my career made another step change into the creation of new environments, which I describe below.
Academic
Academic environment is a haven–harbour, place of safety and refuge, providing and sustaining a home base and favourable opportunities for explorers. It is a place where ideas and idealists find their home, and my perception of this environment is idealistic in nature.
Academic departments are harbours of academic life, dotted around the coast of the sea-faring island that is the institutional home in which they belong. Harbours face different seas, build and sale different ships, and require different captains and crew, tuned to the weather and missions they undertake: the small fishing harbours of Devon of my childhood holidays, the base, now, of highly systematized trade in large amounts of fish; the shipyards of the north that I spent time in, in my industry days, producing and servicing naval vessels for defence; the trading ports of the east coast ferrying containers from suppliers to markets; the transport hubs of the south-east coast, running ferries to and fro to the continent; the sailing marinas of the south-west, homes of sport and leisure.
Academic harbours connect across many disciplines and domains and their missions interconnect. The academic harbour masters must look inwards to support the needs of the island and outwards into the seas of discovery and endeavour, on which they and their members sail. Some succumb to the lure of the sea and tend not to see the community, harbour and island behind them, where they are based. They lose connection when they cast off their boats and take for granted the support and constraints of their home base. Some find it no longer there for them when they need to return and may sink at sea. Some stay land-locked and never sail.
Balancing these perspectives is crucial and is the responsibility of the academic harbour master. In a new harbour, which must make necessary new connections with other harbours, some of which are likely resentful and fearful of loss of trade, it is a considerable load. Making connections that help make this new harbour a haven is hard work–onerous if it fails and a privilege and joy when it works out well. It is up and down in real life. Academic harbours thrive as a balance of support of their parent institution for distinctive discipline and mission, freedom conferred on the harbour master to frame and pursue that discipline and mission, and capability of the different captains and crews, and their ships based there, all drawn together into a distinctive home base culture, environment and trust. The ships and their captains and crews earn their reputations at sea and need the port for shelter, sustenance, regeneration and repair. The harbour is a home base. It is where ships are built, and teams and teamwork grow. It is a place where trust can grow and must be continuously renewed, and nets repaired.
The spirit of adventure, connection and trust was what underpinned my efforts on being head-hunted in 1995, to create and lead an innovative new academic centre at UCL, to be established on the Whittington NHS Trust site as a department of the Medical School of UCL, at the time of its merger with the Royal Free Hospital Medical School. This harbour was to be the home base for three founding and complementary flotillas–health informatics; medical and multiprofessional education; and health services research. The seas they encountered, nearby and further away, were usually quite stormy! I reflect further on this experience, in the section below about creating new environments.
Public Sector
My experience of the wider public sector came in part from becoming involved as a volunteer, in managing the Churches Housing Association in St Albans. The interaction with national policy and institutions like the national Housing Corporation, and their regional governance structures and networks, provided me with insight into legislation, the bidding process for funds, running building projects and maintenance services, and their financial management. The most important experience was the weekly interaction with tenants and the complex network of support agencies that those in need had to negotiate. It illustrated the fragmentation of care services, among multiple competing and discontinuous agencies, much as Bob Jones had focused in the ConCaH charity that I described in Chapter Seven–all requiring and suffering from lack of good interface of public sector and voluntary sector engagement and governance.
I continued to experience the public sector in many other guises, throughout the era charted in Chapter Seven–covering the interaction of information technology with health care policy and practice of the past fifty years. I saw at close quarters, many agencies involved in health care, at the local NHS level in London and on a national scale, in matters of finance, contract, infrastructure and operations, spanning from ministries in Whitehall to City Livery companies, professional bodies, governing boards of NHS Trusts, research funding agencies and research institutes, charities, publishers and national libraries… The emerging health informatics domain connected throughout–truly a Whitehead anarchy of transition!
Commercial and Industrial
In my first post after university, I experienced environment and community of largescale industrial engineering production, contract, finance, project control and corporate management. This was, at one time, where I had expected to pursue my career. But the career path ended abruptly when the group of companies I had joined landed me in a dysfunctional commercial environment. Large amounts of corporate money were piled as chips, staking misguided corporate ambition, fuelled by hubristic promises of technological innovation in medical engineering that came to grief a few years later. The experience of this environment gave me the eyes to see, in later years, at a senior level, how the NHS mismanaged and repetitively came to grief over policy for information technology. Luckily, I was able to change course and head to the starting gate of academic computer science and medical computing at UCL, and its teaching hospital, UCH.
The hugely successful entrepreneur Hermann Hauser was involved in the early stages of the first UK school microcomputers, developed at Acorn Computers in Cambridge and in partnership with the BBC. This was the BBC Micro, and Hauser became a very rich venture capitalist, in taking the technology on much further. This led to the reduced instruction set computer (RISC) architecture machines and micro-processors at the heart of many mobile phones, and the ARM company, globally. My wife and I received social invitations to celebratory events–an Acorn Computers company sponsored concert in King’s College Chapel at Cambridge, hosted by its CEO, was a memorable such event. In my work on educational computing, I came to the notice of major publishers and computer manufacturers, dipping their toes in the sea of informatics and its potential in their different domains.
From Cambridge at that time also arose Autonomy, a talisman of AI arising from a collaboration of computer science and text processing researchers in the University. It was where Mike Lynch was gaining traction in devising algorithms for machine learning, parallel to the rise of the Google pioneers at Stanford University. Google was an Information Age phenomenon that ballooned to become a new globe. Autonomy bubbled and burst. I had heard a bit about its rise through a partner in its parent Venture Capital company Apax Partners, John McMonigall. We were both Trustees of the StartHere charity, along with a board of industrial, commercial and legal titans and a young team of immense devotion and dedication to its cause. StartHere features as one of the examples of creation of new environments, below.
Charitable and Voluntary Sector
The voluntary sector has provided some of the best examples I have experienced of good environment. Where participants feel motivated to offer themselves and their time, freely, there must be good and resilient qualities in play, united in shared values and mission. As mentioned above in connection with public sector environments, for ten years I held office in a local Churches Housing Association. The stretch to provide daily shelter for the homeless and accommodation for those unable to purchase homes, within an umbrella of public finance of building and benefits agency support of tenants in financial difficulty, illustrated the breadth of disconnection between public and voluntary sector services. The gap between services and needs is often bridged by the local generosity and goodwill of those able and willing to volunteer.
A decade or so earlier, in the late 1960s, I had been a member of the British Executive Committee of the fledgeling Amnesty International, in London, encouraged by my late father-in-law of the time, Eric Baker (1920–76), the co-founder of Amnesty with Peter Benenson (1921–2005), and the Campaign for Nuclear Disarmament (CND). In Amnesty was illustrated and exposed the immense solidarity and commitment of communities thrown together as exiles from war in Europe, towards concerted action in support of those imprisoned for their bravery in speaking out against oppressive governments.
The breadth of wider community support for this activity was revealed in fundraising events in the City of London, organized by supporters. A concert at which The Amadeus Quartet played for us (themselves and their families motivated by experience as wartime refugees) drew an audience connected widely across local communities, commercial and public sectors, professions and politics. The Lord Chancellor, Gerald Gardiner (1900–90) spoke at one such event. A future Solicitor General, Peter Archer (1926–2012), chaired our Board–I started there to see the workings inside Parliament.
The global work of Amnesty of that time combined synergistically with the mobilization of local support groups in concrete action to maintain communication with, and support the families of, those imprisoned. It showed how global mission and local mission could be connected in concrete action that anyone, thus motivated, could engage with–fundraising, letter-writing, sending food parcels, campaigning. This synergy did not rest on local actions of national bodies, but did rest on their global agreements, as expressed in the UN Declaration of Human Rights. Maybe there could be models there for global and local governance of the care information utility. There would be much less of a political overtone to such governance arrangements, I feel sure.
Community Interest Company
The coherent interface of health care information as a utility, with individual citizen, local community, profession, organization, business, technology and voluntary sector, is a circle that must be squared within conducive environment and governance. We have evolved utilities of water, electricity, telephony and broadband. We need an evolved coherence of care information as a utility, too.
Stephen Lloyd (1951–2014) was a Quaker lawyer who helped to modernize the charity sector and conceived the idea of the community interest company. I first met him when we were Trustees, together, of the StartHere charity, which I describe below. He advised government and pioneered changes in Charity Law in the UK, to align public, private and voluntary enterprise, to promote new ways of working together, based on sound economy, and squared with the pursuit of shared goals of common interest in wider community. Thus arose the legal framework of the Community Interest Company (CIC). At its centre is the concept and guarantee of asset-lock–shared ownership of community assets and the co-creation and governance of community enterprise, wherein all partnering sectors share roles and responsibilities. Very sadly, Stephen died in a sailing accident, a few years later.
Stephen’s law practice, Bates Wells and Braithwaite, and his successor there in supporting Community Interest Companies (CIC), Abbie Rumbold, played an invaluable role in supporting me to translate the UCL-anchored mission of openEHR into the openEHR International CIC, in 2018. My anchoring support at UCL came throughout from Cengiz Tarhan, Chief Executive of the UCL Business organization and a long-term, invaluable and trusted colleague. OpenEyes had followed the same route and Peter Coates (the founding CEO of the Apperta Foundation, which took OpenEyes under its wing), along with Bill Aylward and my openEHR Foundation colleagues Ian McNicoll and Thomas Beale, and EU colleague, Gunnar Klein, supported me hugely in this process. This two-year period of legal steps, consulted on throughout within the increasingly worldwide openEHR community, brought into being the Community Interest Company structures through which the IP-owning openEHR Foundation and the self-governing operating company, openEHR International, now exist.
Cost-Plus Environment
During my early career in the 1960s, major public projects to construct national infrastructure and complex systems, like warships, were handled through what were called ‘cost-plus’ contracts. This was implicitly a sharing of risk, much as the rapid production of the Covid vaccine, at scale, was negotiated in the UK. Unpredictable and potentially costly risk carries a high commercial insurance premium. In large institutions a choice may be made to carry the risk internally, avoiding payment of the premium but at further risk of carrying the larger loss, should it be incurred. Large shipping fleets were sometimes not insured, where the wealthy owners (the Onassis’s of the shipping world) could cover, internally, the costs resulting from the occasional sinking at sea.
The building of warships at Barrow-in-Furness was where I saw cost-plus in operation. A meticulous internal process was set up and funded to enable focus on quality of manufacture and to minimize the risk that the project would not be completed as planned. The government accepted these costs, subject to its own independent and ongoing review of the manufacturing processes. The shipyard got on with building the ships and submarines, relieved of the concern about financial consequences to them, should the uncertain innovatory nature of the project delivery run into unpredictable difficulties.
Given the extreme emphasis given to supposedly rigorously risk-managed contracts for the National Programme for IT, and the considerable associated cost and furore arising from its subsequent failure to deliver, one wonders whether a more rigorously monitored cost-plus approach might have both delivered much more and cost much less. It is arguable that limitations lurking under the bonnets of the products and services purchased could, much more readily, have been revealed and managed that way. Of course, this would have required a different culture and competence of purchase as well as of supply. In earlier times of innovations of physics in medicine, the NHS valued and invested within hospitals to create and sustain that kind of in-house competence. A culture of purchase contract that encourages hubris, pretence and protective overcharging is not a harbinger of good environment for achieving quality of product and trust in outcome, in complex and uncertain domains of innovation spanning the public and private sectors–and so it proved in this case.
Creating New Environment
Creating the future is about creating new environments that are adaptable and aligned with new purposes and goals. I have been closely involved with three such endeavours during the second half of my career. Their stories reveal patterns that reinforce one another. They have led to wide-ranging impacts, although their innovative and creative phases have now passed into history. I reflect on these experiences, here, and how they connected along my songline.
The StartHere Charity–Signposting to Services in the Public and Voluntary Sector
Originally founded with support of the British Telecom corporate giving department led by Richard Worsley, and pioneered and inspired by Sarah Hamilton-Fairley and Richard Crofton, StartHere set out with the mission to bring order to the ballooning and cross-cutting domains of citizens advice and support services of the Information Age–every sector creating its own brands and initiatives, all focusing on the same population. For some years, I had been discovering that the fragmentation resulting from the poor connection of a plethora of different public and voluntary sector services, all working with the same clients, was frustrating, wasteful and confusing for all concerned. Dependence upon pervasive but non-coherent IT systems and services, seemed, if anything, only to be making matters worse! This had been illustrated by my work with a pioneering West Country GP, Bob Jones, on the Marie Curie Foundation Cancer Patients and their Families at Home videodisc-based educational resource, and in his ConCAH initiative, as described in Chapter Seven.
Sarah and Richard had previously created a small company called Whitewater, providing marketing and public relations services. They knew well the arts of communicating with wider audiences. The StartHere charity created a unique brand with the strapline, ‘Where to go when you don’t know where to go’. It was an outstanding, but sadly ultimately unsupported, initiative to standardize the signposting of citizens to high quality help and guidance, throughout the voluntary sector and local authorities. My connection with this endeavour provided fascinating insight into the interplay of voluntary-sector charities, national and local government, industry, and the legal profession.
Founding members of StartHere, like Sarah Jane Vernon, had worked with Esther Rantzen in creating and running the widely applauded national Childline charity. The StartHere office, with its highly motivated team and governing board, drawn from a wide and complementary range of communities and joined together by a common vision, was a memorable environment and provided a thought-provoking experience. Over time, they strongly influenced my ideas about care information utility. Sarah Hamilton-Fairley has, and demonstrates to wonderful effect, the most outstanding networking and humble leadership skills one will ever come across, and Richard was stubbornly insistent and persistent in piecing together the technology team. Theirs has been a great alliance.
Together with Richard Worsley and several others working in influential commercial sector roles they drew luminary figures from industry, finance, law and public service onto their board. They won grants and created the StartHere team and environment, in stages: collecting and standardizing information about services and advice, connecting across the voluntary and public sector, prototyping and evaluating the use of free-standing kiosk terminals for use in libraries and at other publicly accessible sites. I first came across their radar at an event hosted by the Nuffield Foundation, to bring together a network of people working across health care and IT communities. I became one of their early targets as a Trustee and was ‘lunched’ by the chair, Richard, and Sarah, and asked to join. I am very glad I did–it opened many doors for openEHR through its formative years, as described here.
Sarah is a most capable and charismatic social entrepreneur. She creates and leads great teams, of all ages but uniformly young at heart, raising money very widely, engaging politicians and journalists, drawing together and cajoling a wide-ranging group of Trustees and supporters–among them, board level members of companies, consultancies and social enterprises. The charity succeeded in pilot projects. One of the first test sites was in the early 2000s, in the outpatient department at the Whittington Hospital, where I was then based with CHIME. Matthew Bond, a health services research lecturer and colleague of Ann Bowling , helped to evaluate its use.
Through my membership of the StartHere board, I gained awareness of the intellectual property law expertise of Oliver Bray at Reynolds Porter Chamberlain, who assisted Sarah, Richard and StartHere on IP matters. Oliver generously held my hand through the legal shaping and assignments of IP to the openEHR Foundation.
The entrenched and muddled bureaucracy characteristic of the domain that StartHere had sought to standardize eventually defeated Sarah’s energies. StartHere had to close, and its wonderful team dispersed. StartHere mission’s loss was OpenEyes’ gain and Sarah helped Bill Aylward and me to stabilize OpenEyes through some destabilizing times, associated with unfortunate disturbances in Moorfields management that interrupted its development for a while. Sarah became frustrated, as did Bill, with the politics there and moved on to work with one of the other trustees of StartHere, Richard Harris, with whom she joined forces with Ron Daniels, a charismatic intensivist, to transform the national Sepsis Trust into the powerhouse national campaign it now is. In five short years, the talents of this triumvirate and their board and team have catapulted concern for sepsis into public awareness and action. Just look at the website to see what they have done–generating publicity, fund raising, action plans, volunteering, support of victims and more.60 This is a tribute to their combined knowledge, ability, savoir faire and determination. A triumph of the new environment that they created and led.
In Sarah, such power was born from honour to her beloved dad, who was very briefly also my colleague in the mid-1970s at Bart’s–he at the height of his professional eminence and me in my early academic post. He was the oncologist Gordon Hamilton-Fairley (1930–75), who was killed accidentally while walking their dog, by an Irish Republican Army (IRA) bomb placed near their home in London. Sarah was still at school. He is commemorated in a plaque in the crypt of St Paul’s Cathedral and her family gathers there, each year, to remember and celebrate him. Her life and career, and its connections, are an amazing parable of where innovation and leadership come from and how they are expressed in the teams and environments they create. It was through the connections I made between openEHR and StartHere, that the idea of care information as a utility started to take shape in my mind, ten years ago.
Clinical Skills Centre at Bart’s–Clinical Skills and Informatics
I told this story in outline in Chapter Four, in the context of my career shift from mathematical modelling of human clinical physiology to the standardization of digital health record architecture. Here, I discuss it in the context of the creation of a new environment.
In the terms used by Kahneman, Sibony and Sunstein, clinical judgements are noisy–level, pattern and occasion bias and noise prevail in the judgements of individual practitioners and their coherence among different groups and populations of practitioners.61 In their final examinations, medical students, all highly intelligent cohorts, must perform prodigious feats of memory, rehearsal of theory and demonstration of practice. The validity of the assessment of this performance has itself been the subject of long-standing assessment and debate. Is a method of assessment relevant, reliable and reproducible, measuring the right things consistently over time. How does the dialogue of teacher and learner review, reflect and respond, to promote learning? In improving assessment methods, the mantra is to reduce, refine and replace. The three R’s of primary school learning (reading ’riting and ’rithmetic) have ramified into these three more threes of R’s to govern assessment, learning and improvement! A complementary trifecta of tripods, again!
In the late 1980s, two schools of thought arose in medical and nursing education, recognizing the increasingly team-based and multiprofessional culture of clinical practice and the need to create a correspondingly balanced and interprofessional environment for teaching clinical skills. The two collaborating Deans at Bart’s at that time, Lesley Rees (1942–2022, the first female dean of Bart’s Medical College) and her counterpart, Sue Studdy, Head of the Nursing School, asked me to take a group to Maastricht University, to observe its pioneering work on skills laboratories and then create something similar at Bart’s. Its motivation was to be twofold. First to gain a handle on a more objective approach to assessment of complementary clinical skills, in the curricula of clinical practice, and second to build a bridge between medical and nursing education. My role in leading the implementation team was to bring senior professional staff from both institutions together within a shared mission, chair and broker the planning process, accountable only to the two Deans, and help build a productive working environment in which to explore cooperation and collaboration.
I was probably thought a good candidate as I was neither doctor nor nurse, but was diplomatically and culturally attuned to conducting myself, often as a peacemaker, or insider mediator, perhaps, in areas of potential tribal conflict. I was never going to make it as a high-profile leader! My style always flew below the radar, and the team around me included some who much better attuned as high-flyers in high-profile leadership, as is needed at the top! Leaders who fly below the radar may, incidentally, be no bad thing when tackling wicked problems, where tribes of complementary perspective, and their leaders, often do battle. Working as an outsider and on the margins was what I had been used to for much of my life–as a child in a children’s home, a country boy at the University of Oxford, and in the marginal domain of medical informatics.
There were also significant benefits, for me personally, in being cast into this new leadership role. My position for twenty years in the Bart’s Medical College had always been side by side with clinical professionals and their everyday health care practice. These developing relationships afforded me uniquely adventitious opportunity as well as important insight into and feel for the ambivalences and ambiguities of health care services. There was, however, a double edge to this position–one of personal isolation, and this had also made it uniquely challenging, given the breadth of mission I had undertaken.62
With Lesley Rees and John Dickinson, we recruited Jane Dacre, and Sue Studdy appointed Maggie Nicol. Together with other colleagues, we formed a small team to plan and implement a joint medical and nursing Clinical Skills Centre at Bart’s. Jane had been a junior doctor with John Dickinson and was pursuing her specialism and research in rheumatology with Ted Huskisson, at Bart’s. She came from a medical lineage; I remember her father, an anaesthetist, who had an office in the adjacent Surgery and Anaesthetics Department, in my earliest days working on the top floor of the UCH Medical School, experimenting with the PDP-8 computer in the early 1970s.
John Dickinson organized the building and Jane and Maggie pioneered a joined-up curriculum for teaching and assessment of clinical skills. I kept the peace and held things together within and between the two institutions, with the senior faculty on the project committee. In practice, we assembled a good team, in a good environment, and they led, and held, themselves together!
The project was a success, the Skills Centre created a first of its kind and, thanks principally to Jane and Maggie, the progenitor of many such resources, nationally and internationally, thereafter. Clinical teaching now makes use of clinical skills laboratories and associated models, simulations and standardized assessment methods, very widely. The environment we co-created and managed was a safe harbour where Jane and Maggie could create and grow into captains of their ships. Jane’s ship was the development and enactment of Objective Structured Clinical Examinations (OSCEs) which sailed through the world of clinical examinations from those days. It is a fond memory to recall her ringing the skills lab bell, to sequence students from one OSCE station to the next, in their assessments. Her personal skills–honed, no doubt, in the highly competitive worlds of television and newspaper journalism and medicine, that she bridged in life–brought her great accomplishment. She later came with me to UCL, both of us having trained there–she as a medical student and me as a PhD student. There she established a Clinical Skills Centre for the new combined UCH and Royal Free Medical School, at the Whittington Hospital campus, under the auspices and protection of its Vice-Dean, David Patterson, who I worked with closely during those years, to create the CHIME harbour that I describe next. Jane took her work into the examinations of the membership of the Royal College of Physicians, alongside the medically trained psychologist, statistician and medical education researcher, Chris McManus. Chris became a joint member of staff between the Psychology department and CHIME. He was feisty, determined and no sufferer of what he felt foolish or unjust. There was occasionally some mayhem!
The Skills Centre was a creative environment–based on a culture of shared endeavour with a clear goal, and set within a wider long-term mission, enabled and supported by the two institutions. It was a springboard of new careers. It also provided an environment to bring together the existing audio-visual and medical illustration departments. For me, it connected with a wider environment that I developed, pioneering computer-assisted learning for the medical students, creating the first networked computer system and support team for the medical school clinical campus, and collaborating with Donald Jeffries and David Perrett in establishing a new biomedical science degree course.
At this pivotal stage of my career, Sam Heard drew me into the bid for the GEHR project, and I switched from my focus on modelling clinical physiology to development of health record architecture, and to establishing my first department, with the small team that had grown around me in the Clinical Skills Centre project. We called it Clinical Skills and Informatics and established it close-by to the academic department of General Practice and Primary Care, as I described as the second of three sliding doors along my career trajectory at that time, in Chapter Four. This new environment was a creative one. The department was closely anchored in the primary health care community of East London, and with local endeavours seeking to improve computerized care record systems, in the pioneering work led by Sam Heard, Paul Julian and Dipak Kalra, as described in Chapter Eight. General practitioners (GPs) were also battle hardened from years of establishing themselves in the hierarchy of academic medicine, much as medicine, decades before, had struggled to establish itself within the hierarchy of academia more widely–surely it was just apprenticeship and trade, was the airy perspective of those days! I am remembering, here, how the then Astronomer Royal, another Airy (George Airy), dismissed Babbage and his computer, long ago, as mentioned in Chapter Five.
GPs were thus great allies through these times, with their implicit understanding of the situation faced by the marginal discipline of medical informatics. This stage of building my new working environment within academic medicine was a battle, pursued on ground where wide-ranging alliances were supremely important.
CHIME at UCL
I wrote in Chapter Four about the opportunity to create CHIME, describing it as the third of three sliding door moments in my career transition of the early and mid-1990s. Here, I reflect on the experience in the context of the creation of a new environment, with a brief to foster connections widely across disciplines, professions, organizations, industries, communities and governance of health care. CHIME was an exercise in creating an inclusive environment, bringing together a team drawn from diverse walks of life and complementary perspectives, joined under a vision and mission of multiprofessional education and health informatics–a conjunction somewhat contrived to spell out CHIME! For whatever reasons–and overloaded expectations of our mission at Archway was, I think, one such reason–the nursing and medicine multiprofessional elements did not gel as well at UCL, as they had done at Bart’s. The story of CHIME is also illustrative of generic and multi-faceted challenges of innovation across boundaries of public and private sectors, locally, nationally and internationally. It illustrates how informatics has become entrained, entwined and confounded with everything! AI, a now exploding domain of informatics, looks poised to become so, likewise!
As a founding team, we were dedicated to and attuned to learning by doing. I am indebted to and celebrate all the colleagues who joined with me along this part of my songline. There were invigorating and significant successes and wearisome struggles and failures, with important learning in all respects. We will all have experienced things differently, learned different lessons and drawn different conclusions. These are my recollections. The account I give does not attempt to cover all who contributed within and in connection with CHIME. It draws on those closest to me in my work and roles as its leader and I have sought to illustrate the wider context and challenge implicit in creating such an environment, which is inevitably an ambitious, risky and contentious endeavour. The trifecta of ambition, risk and controversy expresses a complementarity–such is the nature of disruptive change. Stories from the CHIME years appear throughout the book. They provide an illustrative context for, and examples of, the present-day predicament of our overloaded and, almost intrinsically, messy health care services, and how the computer can contribute to their reform and reinvention for the Information Society of tomorrow.
For as long as I could then remember, dragons of medical politics had been breathing fire as London’s historic NHS Hospitals and University Medical Schools were merged into larger groupings. Weighty lords of the realm did battle within the federal University of London, merging and reconfiguring some twenty separate medical schools into five principal centres. The battles came to a head near to me in the early 1990s, as the venerable Bart’s Hospital, with its close ties to the City of London, was required to merge, reluctantly and sometimes angrily, with the London Hospital in Whitechapel, and their two separate medical schools into Queen Mary College, close by in the London East End.
In North London, one of the new groupings was centred on UCL, where the brave and formidable Provost of the era was Derek Roberts (1932–2021), formerly a titan of the electrical engineering industry. One of the UCL Medical School clinical campuses was in Archway, North London, at the Whittington Hospital NHS Trust. The chair of this Trust at the time was Helene Hayman, soon to become a Labour health minister in the first Blair government of the late 1990s and then leader of the House of Lords. Through the then Dean of the Medical School, John Pattison (1943–2020), and the Vice-Dean at the Whittington, David Patterson, advised by my long-standing colleague, Mark Leaning (who was then based in the Clinical Operational Research Unit of UCL (CORU)), I was approached to bring my team, which had grown together through the Skills Centre and GEHR projects at Bart’s, to UCL. There we were invited to establish a new health informatics and multiprofessional education centre within what is now the UCL Biomedicine Division, to be based at the Whittington Hospital as a joint University and NHS initiative.
These senior leaders were hugely supportive, always, and organized generous funding and wonderful new accommodation for us. David Patterson worked astutely and effectively to fit everything together and make things possible. It was David who christened us CHIME–Centre for Health Informatics and Multiprofessional Education. If ever opportunity knocked, it knocked then! We saw and welcomed the opportunity, trusted as a team, made few preconditions and jumped as a group. It was quite a jump! Bart’s was a bit shocked, but impressed and generous, and wished us well.
Derek Roberts had met and corresponded with me prior to deciding to go ahead with the invitation to our team, and Jane Dacre had held discussions with the Whittington Trust, where she was to become an NHS consultant rheumatologist. I said from the start that I was keen to make the move. Derek then drafted and signed the letters to each of us, individually, as UCL Provost, offering us our new appointments. We did not seek salary increment in the move–that eased the transition. David Patterson later remarked to me that the Provost had been agreeably surprised by the straightforwardness of my response to his invitation, having expected he might have to raise his bid! Apparently, being head-hunted tends to go to the head, and the negotiating tactics of sought-after academics were sometimes aggravating to this former industry titan! The straightforward negotiation helped set us off on a good footing.
The diverse founding team of CHIME had an adventurous spirit in common, honed by some years of working together in different groupings at Bart’s. It included nationally recognized leaders–some already at or near to professorial level–with anchoring in health informatics, medical education, clinical practice and health services research. Together with close-by colleagues in Primary Care, the multiprofessional and interdisciplinary environment of CHIME became a unique and special harbour–not always a peaceful or approved of one, but how could it have been!? It was a home for a creative mix of vivid personalities and perspectives, connecting very widely beyond its base. There was always a Herodotus-style ensemble of contending eyewitness viewpoints and narratives in play, connecting far and wide. CHIME made a difference and mostly survived for the nearly twenty years until my retirement, when it had had its day. Derek Roberts was, from the start, wise and prescient about its mission, telling me that he saw it as disrupting patterns and seeding new ones, and that we should keep it going while it was working and worthwhile, and adapt and change it as times moved on, as they always do. How we tackled its challenges was going to be as important as what we did.
In the summer of 1995, I moved with ten colleagues to begin to create and run this new centre. Those who came with me in stepping through this third sliding door of my health informatics career songline, and those who joined us there to develop and extend it over the following years, have been principal actors and leaders of many of the endeavours that are joined together along the storyline of this book.
My role as the harbour master of CHIME was different from that of colleague UCL heads of department in well-established academic fields and organizations; it challenged me to the core. We had to discover what was needed by creating it, and this was inevitably a highly uncertain endeavour. The brief was an open and formative one–open opportunity, open playing field, but no open sesame! No genie and abracadabra to magic solutions to the sorts of difficulties and ills that our recruitment there reflected as having been rather intractable ones. To address these innovatively, CHIME needed connections with many well-established harbours of discipline, profession and practice, spanning the worlds of medicine, information technology and health care. Some new alliances that we worked on, worked out well, and others did not prosper; everyone tried hard, and variously adjusted, adapted and moved forward.
Marcia Jacks, who had starred as the project administrator with me for the GEHR project, as described in Chapter Eight and a Half, was an amazing harbour manager. Strong and assiduously loyal and determined, she became a trail blazer of good practice and ethnic minority leadership in UCL and went on from CHIME to manage the UCL Institute of Women’s Health. Espy Rodrigues succeeded her as centre manager–sadly dying very young, from cancer, several years after my retirement.
CHIME was never an easy environment, for anyone. In health informatics, alone, there were many and disjoint perceptions about us, and expectations of us, in play. One might parody these as spanning from providing a service to ‘keep my printer working’ to fulfilling a delegated role to ‘create an information technology panacea for the woes of hard-pressed health care services’. Indeed, we needed to help organize much of the IT infrastructure and education facility required for the new Archway campus.
CHIME did, though, provide unique opportunities and we set out to make it a straightforward, inclusive and friendly home, where everyone had encouragement and freedom to lead the pursuit of their interest. I summarize here and in Chapter Eight and a Half some of the connections and contributions made, achieving many kinds of impact and success, nationally and internationally. Of the team that came together in the CHIME environment, there are now more than ten UCL professors or emeritus professors. They found and sustained their own successes in what was both a fertile and demanding environment, as creative environments always are. Two of its clinical leaders went on to become presidents of medical Royal Colleges–of General Practice and Physicians. Others moved into senior appointments and responsibilities further afield.
Leading CHIME through those formative years was complex and subtly hard work, perhaps mitigated somewhat by the experience of coping in challenging environments that had been instilled in me since childhood in a children’s home. Not that any CHIME folk were in the slightest bit child-like! It was a grown-up and adventurous community and attracted adventurous people to it, interested in the adventure of ideas. It had a good balance of age, gender and ethnicity and Marcia, our Centre Manager, told me that the UCL Human Resources department, that she dealt with on a daily basis, considered the way CHIME conducted itself to be a model of good practice–very much an achievement of her generous but firm character and diligence in her work with us all. I also knew, from experience of feeling isolated and left largely to my own devices in my early decade at Bart’s, that a capacity for both alliance and self-reliance matters greatly when seeking to identify and create a distinctive contribution to any worthwhile challenge, especially perhaps one involving wicked problems, albeit that its enforcement on one is not always appreciated!
Leadership in the tackling of wicked problems is substantially about enabling and protecting others, operating below a radar that seeks to probe and interfere from further afield. Strutting one’s stuff above the parapet in such quests tends not to cut any eventual mustard! But great things can proceed from challenging environments, given vision and sense of mission and freedom to pursue it. My approach was to help connect people and endeavours within their multidisciplinary and multiprofessional contexts, enabling and protecting practical engagement as widely as possible across academia, health care and industry. It was a risky and ambitious strategy in almost every way imaginable, and utterly dependent on the encouragement and enablement of successive UCL Provosts, Vice-Provosts, Deans and Vice-Deans of the times. I did my best with what was possible, and our achievements were not without honour!
That CHIME environment has now gone, and rightly so. The people who created it have moved on and their contributions have disseminated to other centres, nationally and internationally, sowing seeds of new environments and endeavours. Some of them engage with me still, today, although as a follower and not a leader, anymore. I am now a more stationary point of reference on numerous new and dynamically connected personal songlines! It seems an important time, now, to reflect on some of the battles that raged around me through those formative years and my connection with them.
Battling Environments
In one perspective, the idea and creation of CHIME was a brave exercise in high-level wish fulfilment! Inevitably, some of the wishing-well wishes were well-fulfilled, and others not so well. At a local level, it was an ambitious attempt to create an innovative and inclusive new mission that would help bring new impetus to the healing of some long-standing institutional difficulties and resentments. CHIME, and especially informatics, found itself at the centre of multiple battles in multiple contexts. Two urgent agendas occupying the UCL senior management team at that time were linked together in the ideas generated for the recruitment of our team and the establishment of CHIME. The first concerned medical education and the second the relationship between UCL and the Whittington NHS Trust.
For the first, UCL was looking to catalyze new thinking and help unite fragmented endeavours that had come together in the successive mergers into UCL of the previous Middlesex Hospital Medical School and Royal Free Hospital School of Medicine. Unsurprisingly, some ancien régime loyalties and rivalries persisted and played out in the manoeuvres of senior staff! The creation and operation of a new merged undergraduate medical education curriculum was a battlefield of disciplines, professions and organizations, as to who would play, how they would play and who would pay and be paid.
The wider clinical relationships between the specialist clinical research institutes and NHS Trusts, by then all closely linked with UCL, and the research teams based there, was another battlefield. And, as in all universities, there were culture clashes and rivalries between clinical and non-clinical faculties–the latter somewhere between envious and resentful of the perceived advantages of income and autonomy that are afforded to those clinically qualified, and thereby accorded practising clinician status and remuneration in their terms of university appointment.
The Whittington’s relationship with UCL and its larger and more specialized UCL Hospitals and Royal Free Hospital NHS Trusts had long been a tricky balance, with sections of the Whittington community feeling themselves historically disadvantaged in terms of recognition and resource. The UCL and Whittington senior management were looking for an initiative that brought new capacity and capability in support of current UCL and Whittington missions, and a distinctive new dimension of UCL academic mission–in our case that being health informatics. There were tensions around this plan among the already well-established academic teams based at the Whittington, with understandable resentment that resources they had long felt deprived of, was being offered to newcomers. This was echoed in tensions among the medical education community members based at the different hospital sites of the newly merging medical school, reflecting again a sense of unjust distribution of resources in relation to contributions made. Such tensions are writ large, professionally, academically and geographically, in hard-pressed universities and overburdened NHS services. And in addition to this, on the Whittington campus academic medicine was part of UCL, and academic nursing was part of Middlesex University, which gave rise to some further interprofessional and inter-university contention over space, status and influence at Archway.
CHIME was variously envisaged as bringing both balm and creativity to these severally connected battlefronts. Hence, in retrospect, how I have jokingly characterized it here as an exercise in wish fulfilment! It was a good example of a Dreaming in the Dreamtime, and that appealed to me. You might say that CHIME chimed in both David Patterson’s dreams and mine! Other battles quickly woke us up!
Computing services for the UCL academic and service departments was another site of rumbling conflict. Large departments, each claiming special requirements, wanted to retain the early freedoms they had gained in implementing their own IT services, and to continue and be resourced to run their own local show.63 Similar battle played out over library services, between departments and campuses. And central university service divisions had battles among themselves, over custodianship of their respective IT systems supporting human resources, libraries, estates, finance and so on. The UCL central Information Services division, run by the redoubtable physicist, Roland Rosner, provided and championed the need for corporately standardized systems and services, as the only sustainable and affordable way to meet the bulk of service requirements. Dependency on separate local teams was inevitably also unsustainable for keeping pace with the rapidly changing requirements of both technologies and related patterns of work. The central IT services were on a torturous uphill path towards a standardized, reliable and serviceable infrastructure for the whole institution. I was drawn into this fray, as well, to help in establishing network connections and library infrastructure for the academic community at Archway and more widely across the very substantial biomedicine faculties and their related NHS Trusts. Biomedicine had by then grown to constitute approaching one half of the financial turnover of UCL. Its power and influence were a continuing source of friction and controversy within this wider community, as life science and biomedicine grew and powered forward in the Information Age.
The creation of a high-profile and innovative new centre like CHIME inevitably disturbed these battlefronts, as it was, in part, intended to. At the senior level, there was hope and expectation of us helping to bridge the multiple divides. But some quite weighty incumbents felt that the Deanery had acted deceptively in persuading the UCL and Whittington Trust senior leaders to bring us in to disrupt their lives; we were not universally welcome! My prior association with some of the senior clinicians through my membership in journal editorial boards–where I had perhaps been seen as a helpful and peaceable outsider–may have somewhat smoothed the pathway. I knew Barry Hoffbrand (1934–2020), a senior Whittington physician, who I had worked with for some years in the Fellowship of Postgraduate Medicine and on its journal editorial board. He was welcoming to me and, given his reputation as an established and opinionated figure in the Whittington medical community, his approval may have helped in assuaging understandable doubts among those who felt David Patterson had been a bit too adventurous in recruiting us there! I also knew Neil McIntyre, a Royal Free Hospital physician prominent in medical education, who also had a strong interest in informatics. He subsequently published a full history of the hospital and proudly gave me a personal copy.64 Neil was quite angry and affronted by what he saw as a disruption of his own efforts, along with Neville Woolf, a former Middlesex Hospital physician, to shape and manage the new UCL medical education curriculum. But he was quite pleased, as well, that I was coming to UCL, he told me.
Given these swirling undercurrents, David Patterson had been nervous when arranging for me to deliver an inaugural lecture at the Whittington before we arrived, with Helene Hayman presiding and many staff filling the lecture theatre. John Dickinson and Lesley Southgate came to give me moral support. I started by recounting my family’s history in connection with the home village of Dick Whittington, which is where my parents met. I used multiple visual aids in seeking to capture and communicate the breadth of CHIME’s initial informatics and education missions (see Figures 9.7 and 9.8): one linking with the changing pattern of clinical skills and practice, and another with the emerging discipline of health informatics. I did not venture too far into how the computer might prove instrumental in a transition from Information Age to Information Society health care, changing the nature and skills of health care and professional practice! Luckily, the lecture was generally well-received, David told me later, although I imagine that it did not, and probably could not, connect or resonate with all.
Fig. 9.7 An early slide highlighting the changing nature and scope of clinical skills and roles. Image created by David Ingram (2010), CC BY-NC.
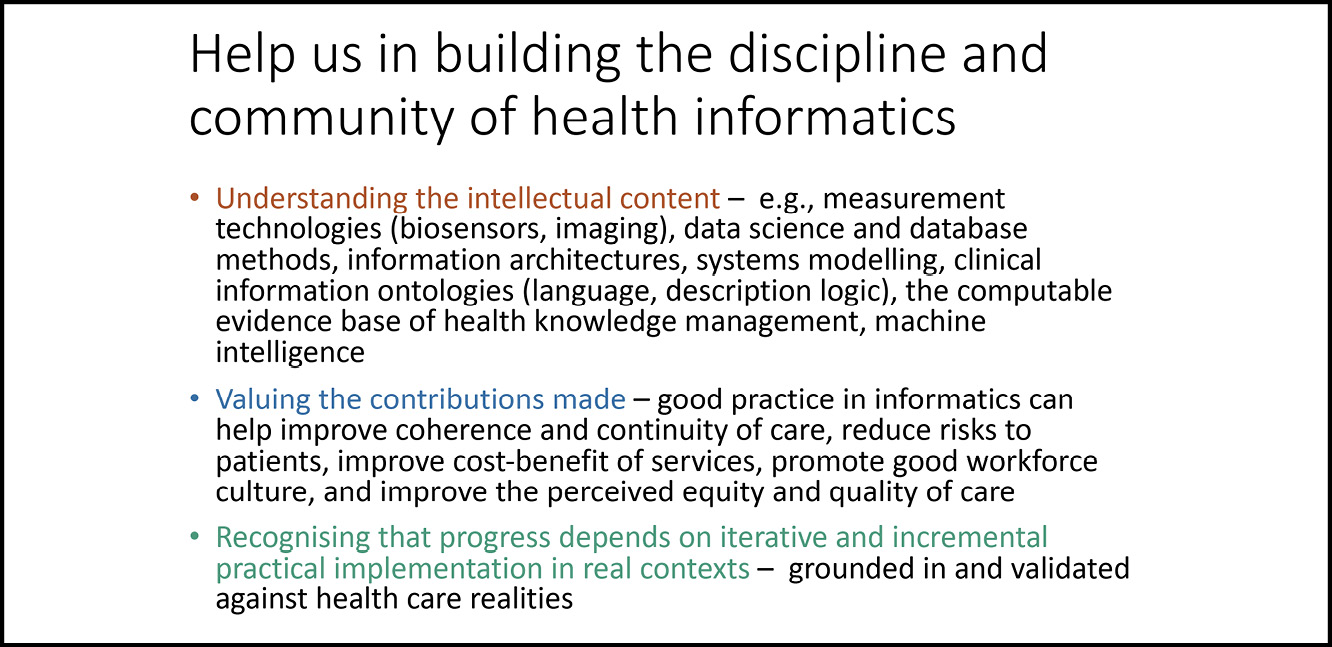
Fig. 9.8 An early slide highlighting the changing nature and scope of care information systems. Image created by David Ingram (2010), CC BY-NC.
And thus, on arriving at UCL and the Whittington, I found myself beckoned and shepherded onto at least four well-defended and contested battlefields, albeit that offensive battle was not my scene or mien! In addition, not far off, and more consequentially for the wider CHIME health informatics mission, were battlefields of health care IT infrastructure and services, at NHS Trust, regional and national levels, and in the interface of NHS and university organizations and communities.65 Finding constructive ways to engage and develop as an innovative academic centre in these battling and divergent contexts, was the brief we had accepted and we gave it our best, although it did not work out well for us all. I could only approach it based on my own understanding and experience, learning how to do it as I went along. I was not about to build walls, install canons and close doors. No one and nothing would have benefited had I attempted to do so, and we would quickly have been closed down, ourselves. I wanted to stay open. That is where I gained traction to open openEHR and work with OpenEyes. Many connections and alliances had to be established and worked on. Great trust was placed in me, and I received invaluable support–within CHIME, locally at the Whittington and across UCL and its NHS Trusts.
The CHIME mission was, and proved, a very big ask, and the answer was only good in parts. We had to pitch tents, simultaneously, on multiple discipline, profession, institution and care sector battlefields! The common ground was one of innovation and change, penetrating across UCL, health care professions and the NHS, locally, nationally and internationally. We were implementers–learning by doing. We were participants drawn into the battles, much more than documenters of the scene. Attempts to innovate in health informatics academic mission, conducted within a clinical academic environment, have been few and far between and usually short-lived. The guns of established rival faculties and departments usually tend to shoot down such upstart startups, within a year or two. We were agents of a higher-level plan, but this did not mean we were, or could be, protected from the heat of the multiple battles! As Sun Tzu would have advised (as I discuss below), this was crossroads ground, and it was imperative to build alliances. I now focus on this aspect of the creation of new environments, with the complementarities of perspective and capability that they express, which imbues them with their strength.
Alliances and Complementarities
Perhaps the anarchy of transition through the Information Age might be described as one of navigating multidimensional crossroads. It switched off traffic lights and left everyone rather frantically eager to get to the other side along their crossing tracks! Moreover, it was a time when roadworks teams arrived to reconfigure all the road! People tend to ride crossly across crossroads, and there are racy behaviours and crashes! Best to organize an alliance and convoy of like-minded travellers.
Our new alliances at Archway, UCL-wide, and nationally, were many and varied and expressed many complementary perspectives and needs. I will give a flavour of them here. They were central to the remit and freedom given to CHIME and its ability to pursue its objectives in academic, professional and health service contexts. My alliances were directed towards connecting more widely rather than digging more deeply, in finding common ground and pursuing endeavours that drew together complementary perspectives, capabilities and purposes.
My foremost alliance at CHIME and the Whittington was with the Vice-Dean, David Patterson, who had been instrumental in our coming there. He supported us magnificently in our relationship with the Whittington Trust and linked his long-standing interest in health informatics with Dipak Kalra and his team, joining in with our European Union research consortia and building systems piloting the Comité Européen de Normalisation (CEN) and International Standards Organization (ISO) 13606 health record communications architecture standard, that Dipak masterminded with David Lloyd (1940–2023). We joined in to support his development of the Archway Campus.
I also quickly sought to connect with the academic primary care community, joining their departmental board, and Jane Dacre, likewise, with the Whittington clinical community. Successive heads of primary care were welcoming towards us–Andy Haines (later the principal of the London School of Hygiene and Tropical Medicine), Michael Modell, Paul Wallace and Anne Johnson (later a trustee of the Wellcome Trust and chair of the umbrella Academy of Medical Sciences) were always supportive colleagues. In due course, Trish Greenhalgh set up her shop just down the corridor from CHIME, as a stepping-stone in her progress to stardom as head of Primary Care at the University of Oxford.
I attended the Whittington Trust Medical Committee over a long period, but I found little that I could connect with in its proceedings, and eventually my membership lapsed. I had many engaging discussions with clinical staff in the Trust, at lunch times. I also connected with the IT department and its heads–notably Glenn Winteringham–became valued sounding boards as we progressed our research on digital health records. We also reached out to Whittington consultants expressing interest in collaboration in health informatics; for example, in the specialisms of dermatology, chemical pathology, rheumatology and diabetes, to explore how these might link with CHIME. Several Whittington staff enrolled on the new and highly successful CHIME health informatics graduate programme, built up and run for many years by Jeannette Murphy and Paul Taylor. Two collaborations that took root and persisted were those led by Jane Dacre, in her dual roles as a Whittington NHS consultant and academic lead on medical education, in the new Archway Clinical Skills Centre, and Dipak Kalra’s with David Patterson and the cardiology department.
David Patterson had long worked hard and skilfully to form win-win bridges with the Middlesex University leadership and its Nursing School based at the Whittington. This aimed at building a new and distinctive partnership between the trust and the two Universities, expressed through joint investment into the new Archway campus development that he masterminded. The Archway Skills Centre, run from CHIME and building on Jane’s leadership at Bart’s, progressed well, as did the library. Our wider alliance with the Nursing School proved more problematic and disappointed expectations, as I reflect on further, below.
Ronald Mason, the eminent physicist chair of the University College London Hospitals (UCLH) Trust of the time, had been warm and welcoming as I set up shop more widely across UCL and its partner NHS Trusts. He invited me to lunch and to talk on several early occasions after we arrived, to help me get settled. Derek Roberts had encouraged him to get to know me. Also, soon after our arrival, the UCL academic chief of medicine, the American renal physician Leon Fine, quickly put me in front of his formidable team, to explain myself. He offered to incorporate CHIME within his huge Department of Medicine. But, having lived in that department at Bart’s for twenty years, I knew that I needed him as an ally but not as a chief. To be seen as a sub-field of his battlefields would not have been a good idea, I thought. There would be one very solid defensive line and ten sharp shooters taking aim from outside! And the internal rivalries of the medicine department would impinge as well–all these clever people would have a view that I should see things their way and prioritize their needs. John Pattison wisely and helpfully confirmed CHIME as a fully independent UCL department, thus giving me copper-bottomed status as my own boss, reporting as Head of Department, directly to the UCL Provost.
Leon became a good and long-standing ally–we were quite different people but got on well.66 He commented once about his bemusement that I remained peaceful and optimistic about chaotic events where he was pessimistic, and his instinct was to do battle! I knew that my mission, if pursued as aggressive battle, would be doomed from the start–I had to embody cooperation and collaboration and a softer and ‘under the radar’ style of leadership. I reflect on the contrast of such styles in the section on leadership, below. I always took on whatever task he asked me to help him with, such as in creating a clinical research network and database of clinical researchers and their projects, across all the NHS Trusts and institutes linked to UCL. As also described in Chapter Five, this was a project developed with Al Aynsley-Green, research lead at the UCL Institute of Child Health at Great Ormond Street. Anthony Peacock in CHIME wrote the software. It was one of several wide-ranging UCL and NHS integration roles that I was asked to take on and oversee.
Further afield I had quickly discovered Charles Vincent and Pippa Bark and their pioneering work on clinical risk management in UCL’s highly rated Psychology Department. Pippa joined us in CHIME, and we secured approval to host her new Masters course. The opportunity to align patient safety concerns with health informatics seemed a clear win-win and a good conjunction to give example to CHIME’s multidisciplinary and multiprofessional mission. Chris McManus in the Psychology Department also worked closely with Jane on assessment methods for the Royal College of Physicians membership examination and we appointed him to a joint post between the two departments.
My CHIME medical education colleagues were also extending their scope and remit. Lesley Southgate had been a powerful figure in East End Primary Care where she became a doughty campaigner in the world of medical politics and ministers, and the battles over the Medical School merger in East London. The health minister of the time, Brian Mawhinney (1940–2019), had himself, in a previous life, been a lecturer in medical physics at the Royal Free Medical School. Building on these connections, Lesley sailed into the world of the General Medical Council (GMC), leading its work on the assessment of underperforming doctors and recertification of doctors’ competence to practice, along with its then President, Donald Irvine (1935–2018). The research team supporting her in this challenging role was based with us in CHIME. It was in an era of national focus on failings in the children’s cardiac surgery department at Bristol and the GP Howard Shipman’s (1946–2004) murders of many of his elderly patients.
Lesley created and piloted the working methods for the GMC and became President of the Royal College of General Practitioners, nationally recognized for all this work in being made a Dame. Unfortunately, she and Brian Jolly had both felt disappointed by their lack of connection with medical education at UCL. Brian quite quickly decided to leave, to take up a position in Australia, and Lesley left much later for a position in medical education at St George’s University of London. One of the principals there was Peter Kopelman (1951–2021), who had briefly worked with Jane and me, at Bart’s, in the era of our Skills Centre project. He had earlier pioneered the Diamond system for managing digital records in diabetes care. In later years he became interim Vice-Chancellor of the University of London.
Bernadette Modell brought the programme of work in her prestigious World Health Organization (WHO) Collaborating Centre for the Community Control of Hereditary Diseases into CHIME. I profile her pioneering contributions in Chapter Eight. One of my subsequent PhD students, Matthew Darlison, was a key colleague of hers in development of an information system for genetic counselling for the community affected by thalassaemia, called APoGI (Accessible Publication of Genetic Information) in conjunction with the haematology service run by the Whittington Trust. This was exemplary in its everyday connections between epidemiology, clinical service delivery and the affected patient community, locally, nationally and globally. Bernadette and some of her illustrious team of professional colleagues from around the world, including Arnold Christianson, from South Africa, became much-valued contributors to our CHIME community. One of her PhD students was leading thalassaemia services in her country.
Jane was appointed to a personal chair in CHIME and went on to lead UCL Medical School. She and her growing team needed to establish their own academic harbour, separate from CHIME. This felt a wrench for me, but I understood the necessity and it worked out well. She took up the mantle of accreditation to practice at the GMC, bringing her Royal College of Physicians (RCP) connections to this. She was later elected RCP President and had a highly regarded reign there, during the height of the tensions, nationally, over the aftermath of the conservative government Lansley reforms of the NHS. In recognition of all this, she, too, was made a Dame.
On his appointment as the UCLH Hospital Trust Chief Executive, Robert Naylor wanted to recruit a previous professorial colleague of his, Paul Bate, to lead a formal programme of organizational development for the newly merged hospitals of the wider trust. I was asked to provide Paul with an academic home and he joined CHIME from Chris Ham’s Health Services Research Centre in Birmingham, along with his close colleague, Glenn Robert, who later became a professor at King’s College. Those sorts of alliances and arrangements were taxing diplomatic and managerial balancing acts–Robert Naylor and the UCL Finance Department had rather different worldviews of the financial commitments and risks involved! Paul connected us with the work of Donald Berwick, a guru of organizational development at Harvard University and adviser to the NHS. Don Detmer, a clinical doyen of health informatics in the USA, became a much-valued member of the CHIME informatics community, while on sabbatical at the Judge Institute at Cambridge.
Among the Deans and Vice-Provosts of Medicine that I worked for was Mike Spyer, who had known of me before I came to UCL, through his research interests that connected him with John Dickinson at Bart’s. He asked me to be responsible for coordinating the merger of the disparate IT support teams in its, by then, fully merged medical schools and research institutes, each closely connected with their local teaching and research communities. I was also asked to chair the UCL-wide IT Infrastructure Committee, overseeing the changing relationship of corporate academic services and academic departments across all faculties, and join the Information Strategy Committee. These two roles were synergistic–to be effective in one I needed to take on the other.
I was asked by John Pattison to create and lead a national academic forum for health informatics, bringing together its leaders from all UK universities. John had by then left UCL, to take on the leadership of NHS Research and Development. He was at that time taking up the reins in framing and initiating the NHS National Programme for IT (NPfIT). In the context of the local clinical mission, I represented the University in its discussions about research that linked with clinical data arising in everyday health care, where there was long-standing national debate about how this could be achieved securely and confidentially. This brought contact with the IT teams of all the local hospitals, in the context of local Trust mergers and implementation of the ill-fated NPfIT. Alongside these ramifying connections, Mike Spyer nominated me as UCL representative on the NHS Modernization Board for London, chaired by Ara Darzi, and John Pattison appointed me to the national NHS Information Policy Board. The interest for me was to listen to and understand what these different groups were facing and what mattered to them, in the context of CHIME’s wide-ranging mission.
On the research funding front, I was asked to participate in numerous activities of the UK Research Councils, involving health and bioinformatics (Medicine (MRC); Engineering and Physical Sciences (EPSRC); Biological Basic Sciences (BBSRC); Economics and Social Sciences (EESRC); Central Computing Laboratory of the Research Councils (CCLRC); Wellcome Trust) as well as the AIM and Framework European Programmes. The MRC appointed me to the national e-Science board overseeing the programme led by Tony Hey, and I supported Christopher Taylor in his efforts to formalize national professional validation of health informatics skills, under the aegis of the British Computer Society. On the libraries front, I was asked to join a multidisciplinary network convened by the innovative and adventurous Chief Information Officer of the British Library, Richard Boulderstone, to consider research information curation in the digital age. From this, the British Library and Wellcome Trust asked me to join and subsequently chair the board overseeing developments linked with PubMed in the UK.
One can see, here, how quickly connections ramify, as a hub and spokes, from a central role in health informatics. They extend within an organization and outwards from it into many and varied academic, professional and care service activities. I treated these as alliances focused on bringing value to UCL and thereby ensuring permission and breathing space for CHIME’s team members to develop their different missions. When Chris Llewellyn Smith was Provost, he awarded me an annual bonus, given to a group of heads of department nominated by faculty Deans. When Derek Roberts returned for his second period as Provost, and with Mike Spyer then as Vice-Provost, they deliberated over my performance in post and gave me a very significant salary increase. Derek expressed his satisfaction with the straightforward way I approached him to review my position and remuneration, when my leadership responsibilities across UCL had significantly grown from those when I was first appointed. But there were disappointments, too, which I now consider, a decade on from the fray.
Reflection
Advances on all sides in the Information Age have brought to the fore the need for new kinds and organizations of health services. These both illuminate new opportunities and add new dimensions of challenge. The creation and sustaining of good environments that can combine learning about new methods, roles and relationships of multiprofessional teamwork, with continuing attention to current practices, is hard work and slowly won. It might ruefully be characterized as a brief to disrupt and supplant current practices without causing too much mayhem along the way! Success in calming such troubled waters depends more on insider mediation at ground level than on orchestration from above.
The ambition that CHIME would help advance the three-way consolidation of institutional missions at the Archway campus in the end disappointed, although there were some considerable successes, as well. Maybe it was too large scale and high profile to take root. Smaller and complementary initiatives might have worked out better and indeed some of that kind did succeed. Notwithstanding considerable efforts on all sides, the significant differences of environment, culture and expectation of the two Universities and the NHS Trust prevailed and persisted. Bridging and healing such divide requires strong and mutually respectful focus, expressed in joint endeavours on the ground, in care services, education and research. David Patterson and the Middlesex University leaders worked very hard to enable this. Matching David’s and Ken Goulding’s high-level investment in that alliance proved a difficult and time-consuming challenge, as it was always bound to be. Nearer to the ground, there was often an awkward mix of personalities and perspectives in play, and, given the diverse wider battlefields across UCL and beyond, on which we were quickly exposed, these sometimes proved more than we could influence, and manage constructively, in a practically sustainable way.
For me, CHIME was seventeen years of citizenship, collaboration, insider mediation and wider diplomacy, enabling and supporting initiatives in many complementary domains through many growing pains and stress tests! Second to alliance building, I knew that sustaining an environment that enabled the careers of teams to progress and prosper, free to martial their own efforts to that end, was most important. This required support and protection, such as I had benefited from in my twenty years at Bart’s. CHIME was both a fertile and demanding environment, typical of any such ambitious and creative endeavour.
A central focus for me, personally, was on achieving technical rigour, clinical and industrial engagement, and wider trust in iterative and incremental implementation and adoption of sustainable methods for capturing and communicating mutually coherent digital health care records. A long sentence, and achieving it a career-long sentence, too! A recognized Grand Challenge of the field for over forty years. The openEHR and OpenEyes communities were created, nurtured and led in the 1990s and 2000s, in the context of my involvement at CHIME and Bill Aylward’s at Moorfields Eye Hospital, as described in Chapters Eight and Eight and a Half. They are CHIME health informatics achievements that will, I hope, remain on the landscape of health care in the future world of the Information Society.
CHIME was fertile ground on which to evolve the health informatics discipline within a robust medical academic community and authentic clinical service context. Jeannette Murphy and then Paul Taylor took on the undergraduate medical education and CHIME graduate programme developments, in close partnership with the NHS’s wider national graduate training programme. Paul was awarded a personal chair in recognition of this innovative educational contribution, and according to today’s lights, Jeannette would have been, too. There is no better way to frame a new subject and learn how to teach it than by engaging with students and learning from them in the process. It is a journey of continuing discovery in a rapidly changing field, to learn how to teach and determine what is important for students to learn. Students and teachers alike have proven to be great leaders on that pathway.
Times changed and when my moment for stepping back arrived (paralleling the situation I had faced when John Dickinson approached retirement at Bart’s), the wide Medical School, University and NHS-bridging roles that I had fulfilled for successive Deans and Vice-Provosts were no longer important and the original integrative mission of CHIME lost traction. Perhaps these different leaders had harboured the expectation that the CHIME mission would be a tide that floated more boats. Our employer was UCL and perhaps I focused too greatly on alliances there. Perhaps we were unable to tick enough boxes of academic and service excellence and impact. In my last years in full-time work, ambitions to establish CHIME-linked commercial spin out companies under the aegis of UCL Business were unsuccessful, resulting in some unhappy frictions on all sides, and I subsequently withdrew from them. There were thus disappointments on several sides in the way that CHIME came to an ending, balanced by pride in our range of significant and enduring achievements, too.
CHIME was a good environment for its time but my efforts to pass it on to successors in defendable shape failed. There was neither the will nor the way for this to happen and it fell apart quickly when I retired from the fray. The reorganization of UCL faculty structure brought Primary Care and CHIME within the aegis of the Population Health Division, and the team moved from Archway to accommodation in UCL’s central London campus. A new and narrower mission of population health informatics inherited its legacy. The wider UCL ambitions for the field that had been invested in CHIME lived on in separate faculty endeavours, where focus was more circumscribed. The health informatics outputs of CHIME were well connected in the world of practical contributions to IT developments and services, but not well in the world of speaking and writing about them. Given the needs and context of the times, this was probably inevitable. Time will tell whether the balance was right. Fortunately, most of my appointed colleagues have prospered well in their new environments and that is good and satisfying. Several years later the Archway campus building, for which we had devoted considerable energy and resource, supporting David Patterson in creating it, was closed down and sold, as part of the rationalization of UCL and NHS estate.
On reflection now, some twelve years later, as I write this section, CHIME proved a catch-22. If we had focused too heavily on a narrow range of activities, the wider community would have likely isolated us as they each had different expectations of the breadth of connection that we had been recruited to achieve. Where we collaborated and connected widely, depth of academic endeavour lessened and communication through publication, that UCL research ambitions also required and expected, suffered.
Implementers on wide fronts are often not people with motivation, time and energy to write at length, as many I profile in this book show. Life is too busy and short for them to do so! More realistic perspective now prevails, in both scope and scale of recognized contribution and output. This would have been more consonant with the CHIME mission, but it was not the culture of its time. It is said that a picture is worth a thousand words. In the context of openEHR and OpenEyes, perhaps their design and implementation in clinical, technical and organizational contexts–and their scaling to self-governing community interest ventures, in a worldwide context, across academia, health care services and industries, over thirty years–may come to be seen as a picture worth more than the thousand journal articles that their creators never wrote about them, or put their names to! I could not do both, as I had been forewarned would prove the case!
On the positive side, from CHIME as a harbour, in its several complementary multidisciplinary and multiprofessional contexts, many sailors found their sea legs, as shipwrights, captains and crew–single-handed and in teams. They learned and practised their craft, built their ships, recruited and trained their crews, and sailed on their different seas. They conducted sea trials near to port, sailed further out and established new harbours, on the same island and as citizens of different lands. That feels a worthwhile accomplishment of the CHIME community and its enablers.
So why does any of this matter and how does it connect with wider issues of health care and information technology? If one travels and experiences the environments of NHS Trust IT departments, as I have done, and connected the story with that of medical physics of decades earlier, as I was also able to do, one sees a concerning pattern:
- Early pioneers developed in-house capability and capacity to innovate within applicable, real-world health care contexts;
- Over time, cost and other pressures led to reduction in these roles and their replacement by a managed outsourcing of innovation in the IT needed to support care services;
- This drew in consultants lacking practical and current knowledge and experience of the delivery of health care, and poorly placed to learn by doing;
- System developers and suppliers were similarly not well placed to understand the changing nature and continuity of everyday frontline health care services that the IT was needed, and expected, to support, from a multiplicity of often conflicting perspectives;
- A focus on watertight contract management compounded the inability to frame requirements, iteratively and incrementally;
- This led to weakened alliances of developers, providers and users of information systems. The squaring of the circle was delegated to a growing market of similarly disconnected consultancy. It is unsurprising that efforts to tackle this both Grand Challenge and wicked problem, have not easily cohered, and their products likewise.
The battlefields of health informatics, both academically and in practical health care and industrial contexts, remain diverse and wide-ranging. They reflect both complementary and conflicting perspectives and drivers and will, inevitably, extend yet further in the coming age of AI. We must continue our efforts to create new environments of community interest, bridging public and private sectors, and encompassing both a vision and the capacity to succeed, over time, in all the complementarities of Implementation One, Two and Three.
New Environment for the Care Information Utility
The previous sections have described personal experience of working in and creating different and complementary kinds of environments along my songline. What makes for a collaborative and innovative environment and how is it created and sustained? And what special qualities are needed for creating environments to tackle radical uncertainties and wicked problems, such as those encountered in creating a trusted and sustainable care information utility, whereby we seek to support the balance, continuity and governance of health care services and what we all do to enable and support them to be good? We must learn the answer to this question by making and doing it. A good environment is, as Wollheim said, a necessity, but it is hard to create and sustain, and easy to undervalue when we have it.
Specialized and bounded domains have a more straightforward task in creating good working environments–their shared vision and purpose is more clearly understood, articulated, enacted and externally validated. Environments that carry the burden of coping with wicked problems have a harder task–here there are often multiple battlefields, and the key is to have vision, discover mission and draw together different threads of leadership, that combine to embrace the wholeness of complementarities rather than exploit their differences. Interestingly, and perhaps paradoxically, the strategy for creating good environments for tackling wicked problems, and the strategy for coping in military battlefield environments, have aspects in common, as I explore below!
The human body has a good internal environment, learned along its evolutionary pathway, that copes as best possible with radical uncertainties and makes life tick. Claude Bernard (1813–78) called it le milieu intérieur and focused on its homeostasis. Body and mind connect and find expression within external environments, both near to and at a distance across the world. We might call these les milieux extérieurs. The two interact and the personal becomes collective, in sharing experience, meaning, purpose and motivation. Life unfolds in environments that are discovered and sought out, created and sustained. Some meet their members’ personal needs and others do not. Experience of external environments evolves along personal songlines of discovery, creation and coping. What makes them good at coping with radical uncertainties and making life tick? Charles Darwin is said to have said of humankind that those who have learnt to collaborate and improvise most effectively have prevailed. Maybe the environments required for reinvention and reform of health care and for creating a trusted care information utility that support a healthy life, should learn from one another more, in emphasizing collaboration and improvement.
A stimulating and challenging environment is fundamental to how we approach the adventure of ideas, cope with anarchy of transition and focus on programme for reform. There will always be both adequate and inadequate environments–nothing is ever perfect and sustaining and improving the environment requires constant effort from its participants and enablers. In learning how to cope with and improve environments that are perceived as bad, or not good enough, we learn to balance our sense of their weaknesses with knowledge about the strengths of those seen as good, or good enough. In both cases, how have they been created, supported and sustained?
Missions make sense when one listens to and observes those who sustain them and ponders how they articulate them. Working environment is a match of the skills and motivations possessed by the teams and communities that populate it and work together on its mission and challenges. Shared goals and fair and inclusive participation are fundamental. Atul Gawande explored the quality of environment in health care services in his book, Better.67 He visited different centres specializing in the treatment of cystic fibrosis, comparing their qualities and achievements. Health care services are not always good working environments–the good ones are held together by their participants as much as their governors, if they are allowed and enabled to do so.
Gawande highlighted good team communication as a key determining characteristic of the better environments he visited. It depends on everyone there, to engender and sustain. I recall reading a similar study in the 1960s, that looked at the quality of nursing care and highlighted the connection of quality of clinical outcomes achieved, such as prevention of bed sores, with the description of the working environment concerned, as reported by its nursing staff. It focused on communication within the nursing team–the more junior staff feeling able to communicate with their seniors. Trust, listening and personal give and take are central to good communication.
Good environments have their day, and their goodness is not solely a matter of narrowly perceived successes and failures in prescribed intervals of time. They may be long-term investments and experiments, with their importance and value slow to emerge, sometimes more widely than within their initially envisaged scope and circumscribed locality. Creation of a good environment is a blue skies endeavour and requires permission, freedom and support in navigating through sometimes stormy seas. Environments collapse, and their participants can be left adrift. Times change and new pastures are sought.
The concluding sections of the chapter look at issues of capability and capacity, connection and community, money, leadership, governance and alliance, required to support and sustain endeavours.
Enabling and Sustaining Efforts
Sustaining mission, environment and endeavour can pose their own wicked problems. Like conducting an orchestra–it is more straightforward when everyone knows the score, but much trickier when challenged with diverse new instruments, music and concert halls.
Capability and Capacity
Creating and working in innovative environments is not to everyone’s taste. It is not a safe or easy life, but it is challenging, and these are places open to creative scope and new discovery and learning. In times of anarchic transition, all environments are to some extent new, although old patterns will tend to persist. The distinguishing feature of pioneers is their joy in the adventure of ideas, in the face of what King called radical uncertainty, and their commitment to programmes for reform. The radical uncertainty of the Information Age exemplifies fundamental issues for health care–about discovery of common ground and teamwork needed for creating and governing a coherent balance and continuity of information.
Key steps in creating a desired future are the identification and growth of the capability and capacity required. These are accompanied by questions about skills and their assessment and accreditation–how criteria are set, and how they are recognized as met. In the world of education, there is continuously evolving dialogue about these issues. In the wider economy of work and service, there are questions about citizenship and participation in the pursuit of common good, and how contributions are recognized, valued and rewarded. These debates have ranged far and wide over the past century–from the writings of Tawney and Beveridge to their successors, today, such as Goodhart, Sandel and Putnam. They resonate through the threads in a braid, as described in the earlier section of this Chapter.
Echoing Whitehead once again, the creation of a care information utility, and the culture it embodies, will best be approached as both an adventure of ideas and a programme for reform. To reform is to re-form–to reinvent and create new forms. In a spirit of re-formation, Goodhart and Sandel argue for radical re-evaluation of how contributions to the common good are judged and rewarded.68 In Tyranny of Merit, Sandel argues that there should, belatedly, be greater humility on the part of winners, recognizing the luck they have enjoyed, and that we need to rethink and not take for granted the role of universities as arbiters of opportunity. In What Money Can’t Buy, he emphasizes the importance of the ability to listen attentively and that this matters as much as the rigour of argument. He argues there for greater mutual respect and inclusion of everyone participating in the ‘public square’.69
These thoughts are echoed in Topol’s landmark book, Deep Medicine, connecting AI with his diagnosis and prescription for treatment of the manifold ills he rehearses of ‘Shallow Medicine’ today.70 In his focus on ‘Care, Period!’ there are echoes of Tett’s alternative AI, anthropology intelligence, as set out in her book Anthro-Vision.71 Putnam’s Upswing is striking in its visual presentation of economic, educational, industrial, political and social data, which exhibit an identical inverted U-shaped curve of progressive convergence from what he describes as the fragmented and egotistical society of the early twentieth century, to a peak of community in the 1950s and subsequent decline over six decades, back to a level of cultural fragmentation that had persisted a century before.72
Leaving aside reward, how will skills, contributions and achievements be judged, recognized and accredited in the building and sustaining of care information utility? In this regard, it is interesting to observe the granular and precise culture that has evolved in the Slack online forum of discussions about physics, for accrediting contributions from among its members. This community exists to provide answers to questions posed by its members. Participants are assessed in a process of peer review in which all members participate–in relation to questions asked, responses posted and how these are valued within the community. It is a carefully categorized process. To qualify those allowed to propose responses to questions, there is a pretest of relevant knowledge and expertise.
In this forum, each question posed creates a new thread of responses, and the questions are also rated in terms of their importance to the community, as evidenced by the interest they generate and sustain. This creates a dynamic environment, adapting in time to the needs of the group of participants–as researchers, teachers, practitioners and students as well. This community is learning how to become open to and inclusive of any participants, but guarded against abuse, misinformation, noise and bias that might be introduced along the way. It prizes authority and authenticity–it is a head, hand and heart appraisal of value of contribution.
The creation of this kind of community is an adventure of ideas. Its purpose is adventurous discussion and clarification of ideas. And it looks to have a reforming influence and potential, regarding the capability and capacity of the community it embodies. I love it–it educates me about an evolving world I once mastered, sadly am no longer capable of fully navigating, but still have the capacity and will to stay connected and informed. Care information utility should, likewise, grow from the adventurous ideas and needs of its participant communities, and will have educational and re-forming influence and potential for health care.
Another area of re-formation is in health care research and development and its translation to and fro with practice. Individual citizen science was very much the norm before the rise of modern universities, where capable minds had the capacity to explore–having means, time and motivation. Universities have professionalized research, but citizen science is again on the upswing, now in more widely connected communities. Tim Spector has in recent times championed this movement in health care, notably with the four and a half million citizens who he signed up to track patterns of Covid infection. I remember him as a junior doctor in the Medical Unit of the Department of Medicine at Bart’s, many decades ago. A remarkable generation of young doctors started their professional careers at that time, in that environment, my close-by colleagues Jane Dacre, John Wass and Ashley Grossman, included.
In well-established disciplines and their well-ordered departments and institutions, there exists a published framework of research endeavours, on which participants and teams are focused. New students are recruited to pursue a topic within that framework. The student is at the outset a trainee in the methods of research appropriate to the topic, and in creating and implementing a plan of investigation. A research programme can still be akin to a bobsleigh ride, a risky and exhilarating experience, but to a largely predetermined and channeled endpoint. The energy, motivation and skill of the rider makes the difference between a slow and bumpy descent and a winning performance, surviving the risks of random over-steering that might result in untimely ejection from the channel! This process risks becoming akin to that of a degree factory, admitting the students at one end of a machine, rejecting those failing quality appraisals along the line, and ensuring that a quality-assured thesis product emerges at the end of the line, neatly dove-tailed with research publications. One view of the product is of a typically little read and unused document. The test applied is that the student has shown themselves able to follow the channel faithfully and reach a prescribed and recognized endpoint. The more important product is a new person–a work in progress in a creative and productive life.
In domains of radical uncertainty and discovery, the attributes of student and supervisor are of a different order. Proposal of a new way of investigating or framing a subject or activity, and making it real, is as likely perceived as heresy or irrelevance as of revelation. There have been examples of this in stories told elsewhere in this book–the computer, prions, bioenergetics, ship design and propulsion! Believe it or not, I have had senior clinicians opine that the X-ray CAT scanner would prove a quite minor innovation! The stethoscope detractors of the Information Age! Heretics are burned at the stake of establishment. Henry Kissinger once said that the reason why academia is cutthroat is because the stakes are so low! The low stakes of well-established discipline do not risk much. Discovery is for higher stakes and risks more. Failure is frowned upon, but some failure is normal and may be protected if the endeavour has insightful and sustained support and patronage.
The relationship of student and supervisor in the uncertain world of discovery is especially close. Two reputations are equally at stake–a trusted or established one and an unformulated one. Unformulated reputations typically grow slowly, on foot, and established reputations depart on a fast horse, paraphrasing, slightly, a well-known saying. In the best of these relationships, the experience is one of catalysis and chemistry, and mutual learning. There is ebb and flow, the supervisor is a sounding board and inquisitor, helping to find productive channels of enquiry, encouraging and drawing the student into them. Stage one is for settling into research method and framing of topic; stage two is discovering that implementation is hard, and progress hard-won. Stage three is drawing together the threads and expressing the results in a satisfactory and examinable form.
As Richard and Daniel Susskind noted, life’s problems do not always fit neatly within province of one discipline or profession or another.73 Where a unifying framework of discipline and profession are lacking, limited or under-developed, goals pursued are necessarily about creating and evolving a new mission, iteratively, through a wide range of initiatives and engagements. The researcher here enters a different environment: one attuned to discovery of the world outside, as an explorer in search of both desired endpoint and route to reach it, as the Stable Diffusions picture in Figure 1.1 of the Introduction so well depicts. Health informatics has been such a domain of discovery, and I was one of the lucky ones enabled and supported to discover, rather than follow a pattern.
Academic identity exists and competes within institutions. Academic initiative in health informatics has been pursued in two ways: as a component of established discipline–computer science, chemistry, physics, biology, mathematics–or as a self-defining and separate entity. By and large, those of the former kind have engaged less widely but survived longer. And those of the latter have had a more exhilarating lifestyle and a more limited lifespan! For me, it has felt more authentic, although personally riskier, for health informatics to be based as an integral part of establishments engaged in health care education, research and service delivery. This provides both an umbrella and a big tent, enabling collaboration between complementary disciplines and professions that are connected there, inclusively, in pursuit of everyday health care endeavours. There have not been so many opportunities like this, and I was lucky to be given two in my career, which made all the difference.
The danger of being based too remotely from the domain being studied is that it risks pointless endeavour. As described in the Introduction, the New Scientist reported on a review conducted by the Cambridge Image Analysis Group.74 They had studied three hundred papers published from 1 January–3 October 2020, on the use of machine intelligence algorithms to interpret chest images from patients suffering from infection by the Covid-19 virus.75 Their stark conclusion was that ‘something has gone seriously wrong when more than 300 papers are published that have no practical benefit’.76 Issues were identified with every stage of the development of the tools. Papers did not include sufficient detail to enable reproduction of their results. Significant biases were identified with the data collection methods, the development of the machine learning systems, and the analysis of results. Little attention had been given to whether these models could pass regulatory requirements to be used in practice. There was publication bias towards positive results. This volume of inauthentic output is noise which risks overwhelming significant, authentic signal of good endeavour and trustworthy and sustainable output.
The extremely low level of what was deemed to be authentically new content of publications in one clinical domain, that I came across in preparing my 1991 Royal Society of Medicine (RSM) talk (see Appendix I of the book’s additional resources),77 seems closely analogous to the situation uncovered in this study. There can easily arise an unvirtuous circle of mutual self-interests pervading research, development, practice, commercial exploitation and publication. It has been evidenced in alliances between pharmaceutical industry, clinical research and publications parading the development and use of new drugs. The marginal efficacy of many commonly used drugs was highlighted in Peter Goodfellow’s Royal Society presentation (he had led on drug discovery in a major pharmaceutical company of the time) that I listened to many decades ago, and again, in recent years, for example in Topol’s book making a case for ‘Deep’ not ‘Shallow’ medicine. Topol adds that ‘shockingly, up to one third of medical operations [procedures] performed are unnecessary’.78 Confabulation among different vested interests led to outcomes such as those starkly exhibited by the congenital malformations associated with inappropriate use of the drug thalidomide. Such black swan events might now be nucleated in careless clinical environments that deploy inadequately accredited AI interventions, adversely influencing human judgements about health care.
A key question is what should a more fully integrated endeavour seek to achieve, and what expectations should be set? I was lucky to be trusted and enabled to set both vision and plan, with the explicit understanding that the successful bits might need to migrate and become rebranded elsewhere, over time, and the unsuccessful bits die away. Taken individually, the outputs of such exploratory and creative endeavours might be deemed to score anywhere between zero and nine, on a ten-point scale. Taken together, they may turn out in the middle and that would probably be a good and fair result. Those who do not risk a zero cannot expect or justify a nine. Scoring all zeros in a real-world challenge is a failure from the outset. Scoring all nines would look unreal.
Connection and Community
Much creativity today resides in teamwork. This flourishes in connected communities and harmonious environments. In my university days, I had the immense good fortune to live and learn about physics in the most creative and connected educational environment imaginable. There, eminent and dynamic people, feted in many different fields of study, walked, talked, ate and rubbed shoulders in everyday life. They brought their global eminence into their teaching within this local community and engaged in their global work from their rooms in the College and in the nearby University departments. They broadcast and communicated their work and ideas, travelling the world to link with similar such communities, near and far. And as the Information Age developed, they collaborated and communicated more widely. It was the quintessence of the Oppenheimer vision of complementarity–people, disciplines and walks of life drawn together and made whole within community and environment.
It was, of course, an elite environment and living there was a privilege. It made me feel elated, after my early life in a children’s home in a rural village, attending a tiny village primary school, and then in difficult, not well-off years of struggle and hard work, as our family moved to re-establish itself many miles away in a city centre. My parents found new bearings in life, and I became good at mathematics at my new secondary school and sailed into University of Oxford, with Cambridge also on offer.
The quality of college community and environment that I experienced, and the luck of being a part of it is intrinsically localized and not scalable. How can the Information Society enable community and educational environment that provides opportunity, motivation, and inspiration of that kind, and enable such experience and enrichment to be more widely, relevantly and justly shared in today’s age, as a young citizen of Globalton? I find it hard to imagine but would hate for such quality of opportunity to be lost. All my recollections of those times are of people, community and environment, and such are uniquely personal, special and unscalable. We need to create more of them. Here are some personal recollections of connection and community, to bear out my comments here.
For example, as I read around for this book, thinking about Chapter Six and the ‘what is’ questions discussed there, I realize it had been a missed opportunity for me, that I failed to get to know the philosopher Gilbert Ryle, who championed philosophy of mind. He was a Fellow of Magdalen College and featured, in my memory, only as a wiry, tall and bald don, of few but crisp words, often encountered walking briskly around Longwall quad to his study beneath my own rooms there, in my second year. There were many such people, eminent in their different fields, who I passed by regularly in my three years at the college and I can see them in my mind, now.
Our physics tutors, James Griffiths (1908–91) and Dirk ter Haar (1919–2002), became akin to colleagues in our small college group of five undergraduate physics students, who studied hard. James had a network from his wartime signals work at the Royal Signals and Radar Establishment (RSRE) Malvern, where he invented a new thermionic valve. This led in later years to his appointment for several years as the vice-chancellor of the University of Malaysia, and then back to Magdalen as President of the College. My special appreciation of Dirk is included in the book’s Acknowledgements. My historian friends at college told me of their tutorials with Alan Taylor (1906–90), historian of the Second World War, Angus MacIntyre (1935–94), social historian of the nineteenth and twentieth centuries, and Bruce McFarlane (1903–66), the medieval historian. McFarlane lived downstairs from me and led a quiet and almost monastic life, with Siamese cats for company. He fitted the image of a medieval monk. MacIntyre, by contrast, was the most avuncular and approachable of dons. Guenter Treitel (1928–2019) was an authority on contract law, shy but smiling to all students he passed by in the College. Taylor was a media celebrity and famed for his ex-tempore lectures that filled lecture theatres. He was a crusty political operator, stirring things up in the senior common room. It was he, thank goodness, that pushed the College to become a coeducational community, doubtless against the terrified reaction of some his comfortably, monk-like bachelor colleagues of the era that I knew!
I got to know these people by a combination of observation in daily life and my friends’ stories of their encounters with them. There were many others, eminent in their fields but just everyday personalities to me–some shy and some noisy, some closeted and some worldly, all no doubt clever and lucky, as we students were, to be there. As students at the College, the quirks and personalities of these teachers entertained us, and their abilities and eminence challenged us. Like the inukbooks on my bookshelves, these tutors were human inuksuks on the academic landscape and the College a memorable place that I travelled through along my songline. The memories of the people and the place, them, echo in my mind as I read about them, and hear stories about them, in later years.
Our student education was built on a rich substrate of people and environment. It provided a safe harbour in which our minds could open, and develop outwards, equipped to sail on the seas beyond. It was hard work, motivating and satisfying. Architecturally, the environment was an inspiring and peaceful place; beautiful buildings, if archaic, and many rooms very chilly in winter; superlative gardens and grounds, with rich wildlife. As a student community, it was spirited and full of life, where social divisions born of wealth and education, mixed with social cultures of students and teachers drawn from across the country and the world. This mixing of disciplines and people made it a magical place and time.
I studied physics and listened every day to lectures from eminent physicists drawn together from the many College communities of the University. This was another kind of local community, interacting around the shared purposes of academic physics, a stage removed from the mix of disciplines in daily college life. And within the University, different departments and fields of study formed another community, this time a local federation, a stage separated from the departments. They were still local, being located within a circle spanning about a mile in diameter. Local colleges, departments and universities joined and ramified within national and international communities and federations, separated by distance and lacking immediacy of connection.
The world moves on and Magdalen is now a different place. The senior common room is the liveliest of hubs and hubbubs, at lunchtime. I doubt that conversation at breakfast is now so sternly frowned on, to assuage monk-like concentration and fragility. They still eat very well but the alcohol is less in evidence! Gender balance is a blessing and after the first female students and fellows of the 1980s, there is, at last, the first female President of College, the lawyer, Dinah Rose.
The Information Age has turned this environment upside down. Telepresence is ever closer and more pervasive. Our physical likenesses, activities, words, records and ideas can be shared immediately to ping and populate devices and screens globally throughout the Internet. The Covid-19 crisis accelerated virtual working community, and physics at Oxford did very well in this. Whereas I would occasionally drive with friends to a Saturday morning programme of lectures in the Department, within more recent times I could enrol and participate in a lecture hosted there and attended from all over the world. Students have worked mainly at home in isolation, with their work supervised and moderated in new ways, by teachers similarly isolated and connected. Recruitment of new staff and students, teaching and examinations, and research collaborations, have proceeded quite satisfactorily, as reported by all involved. In the past week as I write, I have attended a seminar drawing together and discussing with physicists appearing online from the IceCube Neutrino Observatory at the South Pole, along with their theoretical physics team colleagues, speaking from several different countries and a small and very lucky participating audience, including me.
The lockdown has brought some needed gains in the flexibility of systems to cater for the educational needs of isolated individual learners. This adaptation would have been largely unachievable even fifteen years ago, such has been the pace of attrition and maturation of serviceable component technologies. New devices, systems, networks, software and the engineering standardizations that underpin the new skills and ways of working of today, enable increasing alignment within a worldwide ecosystem.
Of course, there is inevitably loss of human immediacy and experience of the academic environment in such rearrangements. This presence has been transferred, with compensatory benefit in family and community life, to local community within our local Globalton. We communicate much more than before along our avenue in St Albans, and through our local WhatsApp group. There is richness of experience and connection to be shared there, that I have previously passed by as I rushed to commute elsewhere for so much of each working day. I have discovered amazing people, hitherto unbeknown to me, living and working nearby. John Snelgrove, an optician and self-made engineer, with a shop practice four hundred metres from our house, has pioneered a technology which may bring personally fitted spectacles, adjusted to personal visual acuity, astigmatism and physiognomy, within global reach for the estimated hundreds of millions of people in the developing world whose lives are seriously impaired because they lack them. And this as a kit and service delivered from the back of a Land Rover or carried on foot, at an all-up cost, including micro-enterprise eyesight-testing and spectacles fitting services, of around twenty pounds! I am connecting him into investment and user communities in Africa, Malaysia and Australia, to arrange pilot production and field trials once his production line is proved and he can produce the kits at scale. Globalton can also be a richly creative and inventive environment!
I formed working relationships from the early stages of my career that can continue, still full of life, now, only because of information technology. This morning, I paused my writing to take a call, screen-to-screen, from Alice Springs in Australia, with Sam Heard, my doctor colleague with whom I conducted the foundational research for, and created, the openEHR Foundation, as described in Chapter Eight and a Half. He is now a medical director for the Aboriginal Community health services, there. Yesterday, I was catching up with work spreading the openEHR open platform for clinical computing across thirty centres of research in Germany. Last week, I was in discussion with a doctor in South Africa, about supporting his pioneering work enabling uptake there of the OpenEyes software for eye care, with which I have been involved for now nearly twenty years. This week, the board of the openEHR International community is discussing with a Finnish colleague the establishment of an educational resource to support education about these new platforms, across countries. These are not unusual weeks.
They are examples of local initiative, enabled by and taken forward within globally extended and mutually collaborative and connected communities and environments of the Information Age. In this evolution, there are new motivations, inspirations, enrichments and satisfactions–and new vulnerabilities, pitfalls and disappointments, too. Money raises its head in new guises.
Money
Money, money, money
Must be funny
In the rich man’s world
Money, money, money
Always sunny
In the rich man’s world
Aha
All the things I could do
If I had a little money
It’s a rich man’s world79
I have not said much in the book about the money required to bring health care into the Information Age–apart from lamenting how much has been and is wasted–aiming high and delivering low. This is in large part a reflection of too much thinking Big, which politicians and policy makers naturally tend towards.
The amount of money required will likely not prove such a central issue once these endeavours are approached more collaboratively, both nationally and internationally, achieving economies of effort and scale. Too much is already spent disjointly and unproductively–the approach of the pioneering initiatives described in Chapter Eight and a Half can lead to massively greater efficiency, effectiveness and value for money, permeating throughout health care economies and across the world. And, as with Arthur Guyton’s (1919–2003) remark to me all those years ago, about research funding, too much can prove as limiting and harmful as too little. Not a popular sentiment among those pitching for billion-dollar contracts, no doubt!
I admit to some considerable cynicism about the role of money in fostering useful innovation. Too little and too much are both bad. Lack of money is seldom a problem for those with power to set goals, borrow and spend. Small budget items, however significant, do not merit their time; they prefer to decide, and act, big, albeit being somewhat prone to missing their targets! Maybe this is because there is bias in their rifle sights, or just noise–upon later reflection, after reading Kahneman’s new book Noise, I am not sure which!
Money certainly matters but a relatively small amount of new money is needed, at risk, if an incremental path of implementation of a citizen-focused care information utility is followed. Each stage can be tasked to deliver sustained value. The work described in Chapter Eight and a Half has arisen and been nurtured with very small amounts of money, capitalizing on insight of a small group of pioneers. It has expended, I would guess, about one millionth of what the world has been spending (implicitly as well as explicitly), year on year, while the wicked problem addressed, overall, has, if anything, got worse. I suspect that is a generous estimate–the real number is probably much higher; we just don’t know how to measure it.
In terms of required information technology infrastructure, the money needed is already being spent, as it has been repeatedly, and often inefficiently and ineffectively, for decades. This money needs to be spent more coherently, realistically and carefully. New investment is most needed to enable and mobilize practical contributions of citizens and health care communities. There are very many capable people in the world with the skills, motivation and enduring commitment needed to weave their part in, and contribution to, the growth and sustaining of the care information utility–the challenge is to create common ground of global synergy from coherent local efforts. I reverse the usual order of such communities of endeavour: motivated volunteers; students of computer science keen for practical assignments in which to hone their skills and experience; citizens eager and able to be involved; health care professionals, technologists, academics, industries ready and able to work innovatively and collaboratively in support.
I have seen this pattern of motivation in several international communities that I have known. We do not nurture and use such complementary breadth of community well–above all, all want to belong, make a difference and be valued. As one very senior friend in international business said to me: making a difference comes to be valued as much as making a dollar.
Leadership
The best ruler is one whose presence is unknown […] When the goal is achieved and the job is done, everyone says, ‘we did it’.80
It is the long history of humankind that those who have learnt to collaborate and improvise most effectively have prevailed.81
This first quotation might suggest that good leadership can prove a thankless task–it may well, in some quarters, but this is not the same as it being unsatisfying or personally unrewarding. Poor leadership is more surely a thankless task, even if financially rewarding. A leader who imposes rather than enables, however wealthy and powerful they become, may likely end up wracked by feelings of impostor syndrome, insecurity and self-doubt. Poor leadership reflects a crisis of values. Poor leadership easily leads to intractable conflict–I saw this in employment tribunals I chaired, seeking to understand and resolve issues raised in complaints from staff.
Care Information Utility is clearly destined to be a very tricky area in which to exercise leadership! Adam Galinsky says that speaking out requires conviction, insight and allies.82 He discusses the range of acceptable behaviours for navigating the double-bind of power, which he sees as: speak too loudly and get punished; keep quiet and remain unnoticed. His proposed tactic: speak on behalf of others, retain no personal skin in the game, keep psychological distance. He quotes Martin Luther King (1929–68) about keeping perspective: ‘don’t be self-focused, find balance in context’. It is a personal matter whether you chose to believe, as he did, that ‘the arc of the moral universe bends towards justice’. It is a sombre caution that ‘we will remember the silence of our friends’.
Good leadership has many threads, not all immediately obvious, balancing individuals with the teams and endeavours they connect with and advance. The Information Age has brought leadership under a new microscope and ‘macroscope’. But the second quotation above is as relevant to ponder today as it was one hundred and sixty years ago. Diverse qualities encapsulate the term: connecting with head, hand and heart; choosing and enabling good teams; imbuing trust, motivation and collaboration; coping with lack of clarity and certainty about goals; discerning signal amidst bias and noise; taking risks in linking people, science and engineering with money–man on moon, nuclear submarine, changing science, changing engineering, changing health care in changing society; coping with irreconcilable imperatives; making itself dispensable; planning for succession…
My former university employer has evolved a clear statement of what it expects of its academic leadership. It is a statement of values in research, education, enterprise and public engagement, and institutional citizenship, emphasizing balance and teamwork. Despots and egotists will fall short of a balanced score card on these scores, however long their list of publications. One publication a year is now considered a norm. Fifty in a career–that fits back to what was being suggested thirty or more years ago, around the time of my RSM talk. The discussion of a career-long evolving account, a songline as opposed to a list of publications, also rings true.
In tackling wicked problems, less is sometimes more. I recall a former Government Treasury Permanent Secretary, George Young, who, when asked in an interview to comment on the main lesson he drew from his years in charge, said: ‘thank goodness we could not do more!’ Focus on individual citizen and population data, on what matters to and what is the matter with, on Little Data in a personal context and Big Data in general, are all balances that care information utility must navigate. We should increment and iterate on these, not follow paths and press buttons that force us one way or the other. Doing too much, at the press of a button, has become all too easy in the Information Age. I recall John Dickinson’s remark to me in my early years as his lecturer at Bart’s, that one of his principal functions as chief of medicine was often to persuade those engrossed in the buzz of the moment in medical science and engineering, eager to do ever more, that they should rather do less!
Leadership in Context of the Wicked Problem
The most difficult situations in which to lead are those characterized by King’s radical uncertainty–where the honest answer is that we do not know but must act, nonetheless. This conundrum lies at the heart of the wicked problem and how we frame and conduct leadership in conditions of shifting sands of both context and perspective, goal and method, ownership and responsibility. These are confronted, and leadership conducted, in situations where no action is an action, no decision is a decision, and where nothing can ever be adjudged right or wrong, perhaps just better or worse, and is either accepted or rejected, leading to further wicked problems.
Leadership here defies rationalization as it arises and evolves within infinite varieties of need and contexts of Open Society, as Popper discussed. In closed society such musings get short shrift. Popper described and characterized the enemies of Open Society. The thirst for certainty opens the door to beguiling and comforting authoritarian siren voices calling for closure. When we stray there, we bring on the clowns, or the despots–sometimes they are one and the same.
Wicked problems can lead to situations where abstract and putative goals predominate, and practical means are in short supply and of uncertain efficacy. Here, connection, listening and being heard are vital qualities, both near to and at large. The solution to a wicked problem is often said to lie in education. But as Norman Davies says, for every person wanting to educate, there are twenty not wanting to learn! The exhortation to educate must in some way balance with capacity and inclination to learn. Achieving this balance requires Tett’s anthro-vision.
Leadership in the interconnected worlds of discipline, Grand Challenge and wicked problem must speak in many tongues. It must nurture trust in its capacity to identify, communicate and act successfully in the challenges of the here and now. It must be versed in the art of war–allies, positions, trade-offs, battles worth fighting. It must build, sustain and define context of endeavour and the teams and terms of endeavour.
The burden of leadership of wicked problems is thus severe, and the hat of such leadership best not worn for too long, as over time it will cease to fit. Leaders must be careful before donning the hat, and remain focused on helping others to share it, and then take it and wear it for themselves. ‘It’s tough at the top’, as every leader discovers, and some quickly find they are unsuited or unwilling to be there, or prefer to critique, or pot-shot, sometimes cheaply, at those who are.
A Songline of Leadership Styles
In the same manner as I reflected above on formative environments experienced along my songline, in this section I set out, side by side, a diversity of leadership styles that I have encountered and worked under.
Chief Executive and Titan of the Shipbuilding Industry
My early experience of the Vickers Group took me to the most unlikely of places, given my home background, but introduced me to some extraordinary and dedicated people, including the barons in that era of the shipyards of Barrow-in-Furness and Newcastle, and the coke-fired furnaces of the steel industry in Sheffield. I met Leonard Redshaw (1911–89) and his team who led the UK Polaris programme to build its first nuclear submarines. He had left school at age sixteen and became an apprentice draughtsman at the shipyard, rising to a knighthood in later years. I saw him at work at the yard, in the two huge, back-to-back offices where he habitually conducted two simultaneous meetings. He moved between them to take charge, sort out an issue requiring quick investigation, issue instructions to the team there, for actions to be completed before he returned an hour later, and then moving to the second office to do the same. Here was an iron and often abrasive will, at the control centre of extraordinarily complex endeavour, showing the prodigious energy that comes when personality and mission match well. He flew and piloted a private plane, to and fro to the Group London Head Office, for management meetings where he represented one of the most profitable parts of the group. He was a gliding enthusiast in his free time. A legendary leader and an astonishing accomplishment, from design and production to seaworthiness trials. But all on cost-plus remuneration, of course.
There I saw how the leadership role and contract was one of balancing expectation, risk and reward. That in contracting for this most complex and uncertain of endeavours, commissioners could not and did not attempt to force all the risk in one direction, onto the organization chosen to deliver on their expectations. This is also true at a more personal level in health care, where there must be a fair balance of expectation, risk and reward, between those who expect services and those who deliver them. This can best reside in common understanding between them, expressing shared values and principles. Lacking such balance, a managerial culture tends towards a spreadsheet culture, abstracting the spreading of expectation, risk and reward, from a human balance to a balance sheet. The dramatic cost inflation of health care services and recurrent failure of its information policy, as exemplified by Topol’s ‘Shallow Medicine’ and the litigation of failures in the UK national programme for IT, are illustrations of where this can lead. It reflects failed leadership of complex and uncertain endeavour. The spreadsheet framing of human endeavour requires little by way of human head and heart, and the computer’s hand will likely do it better!
Chief Executive in the Medical Engineering Industry
My first boss, just for two years until I escaped, was a clinician who switched into medical engineering. He was very bright, ambitious, charismatic and with feet of clay, as it turned out. He established close connections with government ministers and found himself at the centre of the Poulson Affair, where this corrupt architect had spun a web of illicit developments and ventures across the world, especially focusing on new hospitals. Poulson ended up in prison and his business empire collapsed. My boss had run rings around the staid senior management of the Vickers Group, naive in their abilities to switch from military cost-plus contracts for weaponry into a competitive world of medical engineering. They believed in his claimed mastery of a panacea of new technologies for treatment and cure, in the form of hyperbaric oxygen chambers, automation of laboratory chemistry and new hospital design. They backed his dreams and lost a huge amount of money.
It all ended in tears, exposing a dark side of industrial life and international business in the process. He had an unchallenging team around him and those who doubted were thrust aside. Not until the unpaid bills mounted did the group leadership become engaged and they then sent in a ruthless and hard-headed former military brigadier to sort out the mess. He quickly pulled me in to help him understand the problems, which I could readily do, and helped me move away unscathed. Here was my first experience of hubris and pretence of knowledge, and how unquestioningly it is accepted and believed in wider circles.
Head of Medical Physics in an NHS Trust
John Clifton (1930–2023), the Head of Medical Physics at UCH when I worked for him in the early 1970s, became President of the Hospital Physicist’s Association, both in the UK and internationally. He was among the first NHS professionals to adopt this role; it had previously been the preserve of illustrious pioneering academic physicists like Jack Boag (1911–2007) and Joseph Rotblat (1908–2005). These pioneers had worked in biomedical research and its NHS affiliated organizations, to unfold the professional domain of radiation and hospital physics. The field metamorphosed into a wider domain of biomedical engineering and biomedical physics. Heads of such departments had to battle with their hospital leadership for recognition of professional status, tending to be treated as lesser mortals in the ruling medical committees and hierarchies of the day. Hospital physics provided supporting services that were scientifically highly innovative, principally in nuclear medicine, radiotherapy and clinical measurement and imaging services. John was a mix of clever, cunning, motivated and disgruntled. He was a very competent administrator and an effective campaigner on the department’s behalf. He had a loyal, capable, if sometimes rather grumbling, team around him, and the hospital was well served. He exemplified the coping side of leadership–dealt low-scoring cards, he yet managed to win tricks. The world beyond the hospital gave him an environment where he felt more valued, which he surely deserved. He died quite recently in February 2023, and colleagues from fifty years ago assembled at his funeral. He was, I learned there, a lifelong gardener and scout leader. Quite illuminating of his personality and leadership style, I reflected.
Chief of Medicine in a Medical School
John Dickinson was a much more widely known and completely different kind of personality. He played a leading role in the world of hypertension research and was a very insightful and charismatic clinician. He had little time for forceful behaviour, albeit having had a military service period of his own career, and sometimes speaking admiringly of the character of military leadership and discipline. He himself was always sure of his ground on clinical matters but steered clear of personality jousts among contending, more strutting colleagues of the time, charming them with his erudition, practical skills and musical accomplishments.
John was my first experience of a leader as president more than chief executive. He believed his central roles as leader were in appointing good staff to the institution and sorting out their quarrels–quite frequent in the hotbed atmosphere of academic medicine of the era. He believed that his main clinical responsibility was to advise and persuade colleagues when to do less in terms of treatment, rather than more–somewhat counter to the ethos of Industrial Age medicine and the exploratory science of the times.
Vice Chancellor of a Leading University
Derek Roberts was Leonard Redshaw revisited, for me. He was sometimes dour, possessing northern common sense and wielding an iron fist within a variety of determined and persuasive gloves. He was a leader, as Provost of UCL, in two spells from the 1990s and banged heads together with great effect in shaping UCL’s future. Derek was a renowned electrical engineer, who had led the post-war industry that pioneered semiconductor devices. UCL, with all its complexity, was easy-peasy as a management challenge for one as robust as he. He recruited me there in 1995, to create the new CHIME centre in the Faculty of Medicine, linking it with clinical professional education. He described to me his straightforward approach to recruitments to his senior team. ‘Decide what you want to do, locate people who you believe can help you do it and find out what they need’. His disarming, but deadly follow-up line, as he looked you in the eye from across the huge circular table at the centre of the provost’s office, was: ‘so what do you need?’ The approach I took was twofold–express the plan in a simple diagram and frame the ask in terms of the team, not oneself. He liked it and the rest was history.
I reported directly to Derek, as a UCL Head of Department. John Pattison, the then Dean of Medicine, had quickly decided this was the right approach, to give me freedom and keep me out of established departmental clutches! I saw Derek infrequently, thereafter, but he kept in touch and paid state visits to the department. At various meetings that he asked me to join, bringing together leaders from different departments, he came with the aim of encouraging partnerships among disciplines. Equipped with his formidable personality and a single overhead slide depicting an unlabelled set of overlapping ellipses, he extolled a focus on common grand challenges. This he used as his sole visual aid, ascribing the ellipses to different departments and faculties, as he spoke, according to the occasion! This was the most powerful example of intelligent and tough leadership through force of personality and a straightforward, pragmatic approach to management. Mervyn King would have recognized him as an audacious pessimist. I suspect they would have got on well. Derek was a hugely respected power in the land and the successful mergers that led to the UCL of today were his work. His gamble in appointing us achieved and pleased in a lot of ways, and failed and disappointed, in some others. Many years on, during his second period as Provost, Derek and the then Vice-Provost for biomedicine, Mike Spyer, awarded me a considerable hike in salary, so I cannot have disappointed too much! I greatly admired and looked up to them.
Leadership as Battle
Leadership is often seen as doing battle. Two contrasting threads weave together, here, in ideas about battle–one of culture and the other of strategy. One concerns practical focus, as dramatized in the writings of Denis de Rougement (1906–85), which he called thinking with the hands.83 Very French and to be appreciated in that tongue. It has echoes in Goodhart’s book.84 The other concerns strategic focus, drawing from the classically poetic writing of Sun Tzu (544 BCE–496 BCE) in The Art of War.85 This thread is modelled on warfare but generalizes well beyond the military world. The extracts from the book, here, are intended partly as tongue-in-cheek clowning, but, as ever with clowns, with some more serious intent! The book was given to me by my final PhD student, Seref, who is now a humane and battle-tempered, loyal warrior friend!
Denis de Rougemont (1906–85)–Penser avec les Mains [Thinking with Your Hands], 1936
Denis de Rougement was a non-conformist cultural theorist whose views were honed in the interwar years, leading him to strong advocacy of European federalism. It is easy to get a rough translation of his words from Google Translate, but the text only fully connects in its original French tongue! It is a call to hands, not arms in combat!
It is time to proclaim vain any work which leaves its author intact, and the reader to his comfort. Vain and bad any work which does not seize you as with a hand, which does not push you out of yourself, in the scandal or in the joy of your creative vocation.
Too many harmless thinkers conceal correct philosophies, too many harmless dramas are played out in our novels, too many harmless scribes ape us with fury, or revolt, sceptical indulgence, or distinguished peace. Harmless, all those whose work is not the place of merciless combat where something he can no longer flee attacks the author and all that he reflects in a domesticated atmosphere.
It is high time that thought returned to what it really is: dangerous for the thinker, and transformative of reality. ‘Where I create, there I am real’, wrote Rilke. And that is why we will take this distinction seriously: There are men who are the pride of our spirits–and others who pride themselves on our spirits. There are men who create, others who record: they should no longer be confused. There are Pascal and Goethe, Dostoevsky, and Kierkegaard–there are also the literate, the good minds, the teachers, for whom thought is an art of pleasure, an inheritance, a liberal career, or a well-placed capital. Brains without hands! and who judge from above, but from afar, and always after the fact, the multitude of brainless hands who work endlessly through the world, toil perhaps in vain, if not for the loss of us all. Now, these people form opinion, without a doubt, and they know it. All the opinion in the world is pretty much there, that thought can only come after fatal events and which do not care about its stops. It is that we confuse thought with the inoffensive use of what creators have thought, often at the cost of their lives, and always by an initiating and revolutionary act.
Some think, they say, others act! But the real condition of man is to think with his hands.86
A rather dicey translation, but the gist is there. I asked ChatGPT-3 to clarify and summarize the text from Google Translate. It thought for a couple of minutes and then offered the following:
Denis de Rougemont believed that there was a disconnect between thought and action in modern society. He argued that people had become too reliant on technology and had lost touch with the physical world. Rougemont believed that by engaging with the world through physical activities such as craftsmanship and manual labor, people could reconnect with their humanity and improve their mental and emotional wellbeing. He saw this as a way to counteract the alienation and existential despair that were prevalent in modern society. Rougemont’s philosophy of ‘thinking with your hands’ emphasized the importance of integrating the mind and the body in order to achieve a more holistic understanding of the world.
Both are fun to read!
Sun Tzu (544 BCE–496 BCE)–The Art of War
The failures of successive reorganizations of health care have come to look like failed military campaigns. There are those who view government in that way, as afficionados of the OODA loop model of the former fighter pilot John Boyd, which has been influential in some political circles of recent decades. His model of campaigning was based on steps to Observe, Orientate, Decide and Act, pursued with the aim to surprise, and disorientate, to overcome the perceived enemy. This is a strategy that can win the war but lose the peace. It focuses attention on combat over disputed territory rather than collaboration on common ground. Finding common ground rests on strength of arguments rather than force of participants, as well as trust in motivation and fairness.
Leadership of successful campaigns is a cornerstone of military prowess and, to appropriate the sayings of Sun Tzu, from two thousand and five hundred years ago:
War is
A grave affair of state;
It is a place of life and death,
A road
To survival and extinction,
A matter
to be pondered carefully.87
In the one hundred pages of The Art of War, the words are poetic, but the focus is on success in battle of any kind, and best won without conflict. The book is nowadays a standard text in leadership courses, where military battle is used as a metaphor for campaign and leadership more generally in society. We touch on such metaphor when speaking of the war on poverty, want and disease. Language of survival and extinction is staring from the front pages of most newspapers this week, in the context of the crescendo of concern about AI. So maybe our information strategy for health care will start to assume the vestments of military campaign. The strategy for combatting cyberwarfare already indicates this is on a war footing.
The modernization of health care has been a battle and it has certainly been pondered, repetitively, in many different countries and at many different times. It is a battle not yet won. According to Sun Tzu, in combat:
Victory should be
Swift.
If victory is slow,
Men tire,
Morale sags.
Sieges
Exhaust strength;
Protracted campaigns
Strain the public treasury.88
Bill Gates might well approve of this strategy–he has championed the need to take innovation quickly to scale. I am cautious that wicked problems may not be amenable that way. The history of information for health has been reminiscent of a new hundred years’ war and the above extract captures very well the energy-sapping impact it has had within health services.
National Strategies are strategic offensives. In Sun Tzu’s classic, the most quoted and remembered verse is:
Ultimate excellence lies
Not in winning
Every battle
But in defeating the enemy
Without ever fighting.89
In thinking about information strategy for health care, there is no clear enemy, but there is battle, nonetheless, on many levels. And some leaders seem to have fixated on vanquishing perceived enemies more than achieving necessary goals. Strategy is of paramount importance. For Sun Tzu, the highest aim is not to destroy but to overcome by dint of strategy. In this:
The victories
Of the skilful warrior
Are not extraordinary victories;
They bring
Neither fame for wisdom
Nor merit for valour.90
And:
The victorious army
Is victorious first
And seeks battle later;
The defeated army
Does battle first
And seeks victory later.91
This echoes the concern that Douglas Black (1913–2002) raised in his critique of the Körner Report in the 1980s, as highlighted in Chapter Seven, where he distinguished the role of IT in the clinical management of individual patient care from that in the organizational management of health care services. The NHS saw and planned a battle over information for health focused on the latter, consequently neglecting the former. Quiet and uncelebrated progress on the former is a precondition of a successful campaign on the latter. Thus, in the military perspective and language of Sun Tzu, health care got its strategy wrong–it fought on the wrong ground (organizational management rather than individual patient care), divided its troops (managers and clinical professionals), made enemies from friends (IT professionals and the industry) and neglected its allies (citizens and what matters to them). The battle was approached as one of target-driven, up-down taming of professions and organizations by politicians and managers. It has achieved a sickening stale mate. It should now focus on creation of care information utility to serve the individual needs of citizens and professionals and engage and support them in their shared mission in health care, on common ground.
This will be a new battle and will have winners and losers and face concerted battling forces. These comments are not intended as accusatory–all endeavours discussed have predominantly been well-motivated and diligently pursued. But Sun Tzu does find relevance here; and there are several other parts of his epic that should also give pause for thought. Those familiar with the multifarious battles of five eras of NHS IT strategy, seeking towards new equilibrium in health care for the Information Age, may recognize in their own experience, the relevance and wisdom of many of his verses. Here are a few more that struck a personal chord in the context of health care and IT.
The highest skill
In forming dispositions
is to be without form;
Formlessness is proof against the prying
Of the subtlest spy
And the machinations
Of the wisest brain.92
This is advice about staying below the prying radar and avoiding becoming a target!
Victorious campaigns
are unrepeatable.
They take form in response
To the infinite varieties
Of circumstance.93
This is a call to keep in close contact with the uniqueness and everyday unfolding of the battle, adapting to it and not forcefully pursuing a disconnected master plan.
Victory belongs to the man
Who can master
The stratagem of
The crooked
And the straight.94
The challenge is to bring tractable and useful order to an intrinsically disorderly domain.
Leave a passage
for a besieged army.95
In this we must operate inclusively and not punish.
Hence the saying
Know the enemy,
Know yourself,
And victory
Is never in doubt,
Not in a hundred battles.96
As Mervyn King and others have advised, based on their own experiences, we must cultivate greater awareness and humility.
When starting a fire
Be upwind;
Never attack
From downwind.97
And avoid self-harm!
I consulted ChatGPT-3, asking for a summary of Sun Tzu’s message about battle. It was quicker to reflect on this request, and replied as follows:
Sun Tzu believed that effective leadership in battle was essential for success. He emphasized the importance of knowing one’s own strengths and weaknesses as well as those of the enemy. He also stressed the need to be adaptable and to be able to adjust one’s strategy based on changing circumstances. Sun Tzu believed that a leader should inspire loyalty and confidence in their troops by setting an example and treating them with respect. He also believed in the importance of communication and the need to keep one’s troops informed about the overall strategy and goals. Sun Tzu believed that a good leader should be able to make decisions quickly and decisively, but also be willing to listen to advice and consider alternative perspectives. Overall, Sun Tzu’s message about leadership of battle emphasized the importance of strategic thinking, adaptability, communication, and leading by example.
The battle for health care IT has been a multifaceted struggle, involving various stakeholders and interests and unfolding on multiple fronts. The ground-level insider mediation and peace-making now necessary requires a flexibility of approach combined with focus on goals that transcend the battle lines–better balance, continuity and governance of health care. In this, the focus must be on the citizen, not the service.
For me, the most thought provoking of Sun Tzu’s advice relates to strategic alliance. This is the topic I reflect on at the end of the chapter.
Stages of Leadership
Leadership proceeds in styles and stages. Simplifying the description of an untidy world may clarify and represent it well, or alternatively obfuscate and misrepresent it. There are contexts in which the imperative is to close in on narrower goals, and those where it is to open out onto wider goals.
The opportunity of implementation of the care information utility is to combine global and local endeavour. New and worldwide communities that pool their endeavours within new networks of connection and collaboration on common ground. New local community endeavours that inherit approaches and methods globally and collaborate locally to implement in local contexts. Creative contribution comes from all these participants. In the section of this chapter focused on Implementation One, I introduced ideas of Lionel Penrose, concerning human group behaviour. I relate these here to leadership challenges as a function of the scale of team and endeavour. There have been three stages of leadership of GEHR and then openEHR.
Stage 1: 1990–95, Lionel Penrose levels 1–3 and 3–10
This stage is characterized by the articulation of vision: from the formative framing of problems to formative iteration of architecture and design. This stage posed questions about coherence, connectedness and comprehensiveness of requirements, relating to purpose and goal, answering to early questions of what and why?
In this stage, team culture and environment were centre stage. It brought together and united people with clinical perspectives and expertise, already experienced in the world of electronic health records, and joined them with people with complementary technical, managerial and commercial experience and expertise–in small organizations and large. This stage needed to focus on a shared vision and worked from a bootstrap of an already instantiated product, Health One–a concrete example against which to bounce new ideas. An iteration between forward-looking requirement and practical experience and example, looking back.
Stages 2: 1995–2015, Lionel Penrose levels 3–10 and 10–100
This stage is characterized by the articulation and practical enactment of the mission, involving the implementation of test systems, iterating to a refined architecture and design. Here we again encounter the importance of skin in the game in the world of developers and users of systems. If these incremental test systems proved unable to gel and connect, they were unlikely ever to achieve traction and scale in the wider world.
This stage entailed framing the culture of and creating the independent not-for-profit openEHR Foundation under the auspices of its founding organizations (UCL and Ocean Informatics) and assigning all IP to this organization. In turn, a community within clinical and technical domains was organized and built; roles and responsibilities were delegated, seeking traction and momentum, moving out into the wider world, ambitiously.
Stage 3: 2015–today, Lionel Penrose levels 100–10,000
This stage is characterized by a consolidation of the mission: creating and launching openEHR International as a free-standing, self-governing, self-financing community interest company.
Such pioneering is a hard track of endeavour that requires staying power and oftentimes involves considerable personal cost. Throughout, environment, team culture and feasible ways of doing things were fundamental. It is a precarious process to maintain these and remain solvent and true to the culture of the mission, as the scale of operations grows through its early stages. Leadership roles and recognition of contributions gradually become more widely distributed and shared.
Leading from Below
It can be hard to separate leadership and authority from power and position. Articulating and defending mission, creating and sustaining good order, resolving differences and enabling and achieving desired outcomes call on different skills and qualities of leadership, and expose different motivations. Leadership and authority are required and in evidence everywhere. They are not necessarily to be associated with power and position exercised from the top down. Micromanagement is not leadership. People at all levels can be leaders and speak with authority. Leadership may sometimes be best approached from below, as Lao Tzu advised in the quotation that heads this section.
In his 1953 Reith Lectures, which I introduced in Chapter One and have several times referred to elsewhere in the book, Robert Oppenheimer (1904–67) discussed the idea of complementarity in science, and extended this to the human realm and the importance of articulating a shared vision that combines complementary perspectives. He called it ‘common understanding’. This process is one of learning fruitful ways to weave together complementarities, and such are well exemplified by the half and half approaches to and perspectives of health care, as discussed in the next and concluding chapter of the book–fruitful weaving together of human and machine intelligence or health and social care are two pressing examples. We need to learn their intermediation and approach the task from the ground up. Endeavour to create the care information utility must recognize and accommodate this aspect of the implementation tasks. It will require common understanding that guides the inclusive drawing together of complementary threads of implementation. Health care of the Information Age is struggling to achieve common understanding–what it is and what it does. Alongside, so is health informatics. Both have tended to view the quest too much from a top-down perspective of power and position. It is not that this isn’t important; it’s rather that it needs better balance with ground-level and bottom-up perspective of leadership and authority, as well.
UK health IT policy, strategy and plan of action have been found lacking in leading from below qualities, and its leaders have tumbled from the top–the higher they rose, the harder they fell. All sought, bravely, to keep order, stabilize the ship and chart a course, as further described in Appendix III in the additional resources.98 There were the diverse credentials and temperaments of hospital administrator, physicist, IT consultant, IT manager, civil servant, management consultant, journalist and diplomat in these leaders, but very few practising clinicians in sight, and none in this list of those who have led from the top!
But without power and position, will people speaking with authority be listened to and heard? They, too, are leaders. There is conflict as well to be resolved among powerful leaders on opposing sides. In this context, the world at large is revisiting the resolution of difference and conflict, albeit extremely painfully, speaking more, now, the language of intermediation in finding and implementing solutions from the ground up, rather than in high-level power broking. There is discussion of ‘insider mediators’, emphasizing the need for leadership in such processes operating discreetly, below the radar, rather than flying the world in jets, power brokering negotiations, speaking at conferences and giving press conferences.
As outlined above, Galinsky advocates for conviction, insight and allies when speaking out in situations of conflict. His approach sounds very much like leadership from below, the ‘insider mediator’ role. All very well, but it will be a long road to learn and accommodate this leadership skill in the way we do things today, albeit that many parts of the world that have long been embedded in intractable conflict appear to be engaging with it. How could these ideas be extended into health care reform? Only by trying and evaluating their impact can we truly know. Perhaps Implementation One, Two and Three of the care information utility could be one place to start.
As an example of what this sort of idea means in practice, in a completely different and more ethereal context, the Quakers have no priests as voices of power and position–they use poetic language in describing ‘the priesthood of all believers’ and of the spirit (common understanding, perhaps!) as leading. The role of Quaker business meeting clerks is not to lead anywhere, but rather to provide an open environment that enables all those who are present to express themselves. They sit quietly, reflect, summarize and draw the discussion to a conclusion by expressing it succinctly, there and then, in a written Minute, which is read out and approved by the group. I used to sit alongside a famous head of an Oxford College who attended Quaker meetings for worship every week, never spoke there and arrived and departed alone. He was friendly and approachable, though, and no doubt a good leader in college affairs and in the government commissions of the time that he chaired. It seems that, where there is a common ground of purpose, goal and method, a good environment and a common understanding, all who participate lead. He was a national leader who, you might say, was attending there to listen to leadership from below. He didn’t come for peace and quiet as those meetings could sometimes be quite noisy, in my experience of them years ago!
On a lighter note, the leader’s lot was beautifully parodied in the operettas of William Gilbert (1836–1911). I can still hear these being sung, sixty years ago, at the Bristol Old Vic, with the anguished police chief in Pirates of Penzance reiterating many examples of why ‘a policeman’s lot is not a happy one’. But as Lao Tzu wrote two thousand years ago, the best leadership is not seen. There is a huge amount of it in action everywhere, every day and hopefully we can link it better with the leadership we do see. Perhaps good leadership at the top and good leadership from below are another Oppenheimer complementarity, where we either have both or we have neither.
Implementation Three–Governance
Reaching the end of the book’s storyline I come to probably the hardest issue it encounters, that of governance–as if any of it was straightforward! I could have put it first but chose to put it last, as in that way its pivotal position and importance across the domain of care information utility is clearer. Good governance is the storm anchor of trust. It serves to engender trust in and obedience to rules and laws that are constructed and sustained democratically and discharged fairly and impartially. Governance of data and data systems serves to engender trust that data are faithfully, meaningfully, relevantly and securely captured, stored, analyzed and communicated. It needs to protect against exploitation and manipulation by bad actors, too. But badly conceived and enacted governance can be harmful, too. We need to keep learning about how to do it well. It is the third grand challenge of implementation of the care information utility.
Information has causative potential and information governance involves ethics, law and regulation concerned with those causes and their effects. It impacts widely on citizens, services, institutions, professions, industries and governments. It connects closely with information technologies and systems, impacting all aspects of the management and processing of personal data. For example, imposing the requirement that an information system be able to correct wrongly recorded information that is discovered, by tracing back through all the chains of intermediate processing of data to its original source, is a beguilingly easy imperative to sign up to and articulate, but a potentially nigh-on impossible task to enact in the combination of many highly interconnected information systems employed in handling personal health care data, lacking either semantic or technical coherence. To achieve it requires that aspects of the information architecture of the systems be framed around this as a central requirement. It will require rigorous and openly specified formal separation of data from program and application, and for these aspects of the architecture to be common ground across the intercommunicating systems with which the data connects. This makes a formidable case for their standardization, and challenge for their implementation.
Dissonance of theory, regulation and practice embodied in the ecosystem of information governance of personal health data has resulted in an onerous and noisy domain, in terms of what it attempts, how well it succeeds and how it interacts with and impacts on health care. We have dug deeply, over many decades, with ever more penetrating shovels, into a sometimes seemingly bottomless pit of contention about what this governance may mean for management of the complex and wide-ranging kinds, uses and sensitivities of personal health care data. It is hard to broker and reconcile one perspective that holds that personal privacy of data captured in individual patient care must be absolutely assured, with another that holds that free sharing of these data is essential, to benefit both the patient concerned and wider population health services and research. They are both right, in principle, but point in different directions. They are complementarities–two halves that we must make whole. This debate about principles has continued for several decades.
What people say and what they do about these issues matter, and often differ widely. Social media has demonstrated this experimentally, with personal information made freely available by citizens, both in public and to organizations and individuals intent on using other people’s data to serve their private commercial or other ends. Proponents of what should be framed in law and what is achievable in practice, butt horns. Those that value privacy and those that value access, talk past one another. Those that regulate the technology of information systems and those that regulate the performance of information services they support, talk different languages. Those that make money from exploiting personal data, think, perforce, about money.
Such concerns predated the Information Age, of course, but have become amplified by it. What information is being governed and why? Rarefied debate about matters that have not been explored in practice promotes cynicism. I remember the then new Gilbert and Sullivan light operettas, being performed on stage at Christmas time at the Bristol Old Vic in my school days–they were great family fun! There were messages about poorly framed ideas and resulting meaningless words. For example, set to staccato notes that I can still hear:
This particularly rapid, unintelligible patter
Isn’t generally heard, and if it is it doesn’t matter,
This particularly rapid, unintelligible patter
Isn’t generally heard, and if it is it doesn’t matter,
matter, matter, matter, matter, matter,
matter, matter, matter, matter, matter!99
And elsewhere, about support for presupposed conclusions:
Merely corroborative detail, intended to give artistic verisimilitude to an otherwise bald and unconvincing narrative.100
Undue focus on the individual at the expense of the community interest, also exercised William Gilbert:
When everyone is somebody, then no one’s anybody.101
In more serious circles, report after report has pitched successive, and often conflicting, perspectives about Data Protection and the ethical framework that should pertain. Ideas about personal identity and anonymity play out in practical methods for identification and anonymization of data, and in narrow technical and wide philosophical debate.
Kahneman, Sibony and Sunstein discuss pattern, occasion and system noise and how they impact on judgement.102 A key message is that judgement is best treated as a form of measurement, with the same approach to its bias and noise as used when analyzing data. Measurement arose as refinement and extension of human senses. Decision and judgement involve both sense and sensibility. Machine decision making is a refinement and extension of human judgement. In this context, the authors are not yet enthusiasts of machine intelligence, believing that it is going to produce major problems for humanity in the next few decades and is not ready for many of the domains in which judgement is required. The authors assert that good ideas should take twenty years to frame. That used to be the stated timespan of bench to bedside translation of scientific advance to routine treatment. But no longer so, in the Information Age. The problem is that short-term capability and judgement can propel innovation to activation much faster, while its consequences may still play out over the longer previously identified timescale. Does any government or governance process designer consciously think on such timescales now–or can they, even?
We must therefore be very cautious and clear-sighted about the extension or encroachment of machine intelligence into a matter as consequential as information governance for health care. There is already too much noise! In 2023, the likes of ChatGPT are racing ahead of this curve and normally ambitiously disruptive souls are expressing concern, cautioning in favour of the incremental and iterative approach characterized in the quotation from Whitehead that headed this final part of the book.
In Chapter Eight, we looked at information as a monetary system. Citizens and institutions own money and banks provide services to manage money. Governments and central banks protect and regulate the monetary system within national and international law, while many others may seek to game and corrupt it. We need law and practice to succeed in maintaining a resilient monetary system. Mervyn King said we need new ideas about monetary governance. Health care information flows within equally pervasive personal, professional, institutional and government communities and networks. We need new ideas about information governance, too.
Trust in personal ownership of money is fundamental to its value and governance within a monetary system. Otherwise, we would probably revert to barter, token or precious metal as means of exchange. Affirmation of personal ownership of health care data will be tokenism, and will remain so, unless and until we have personal data banking methods, by which we can learn how to operate, govern and regulate these personal data. This will require new focus on information architecture, new technology and new culture of citizen and professional relationship in health care, built on new common ground.
If citizens are to own their personal health care data and health care services are there in support of this personal autonomy, care records, co-created by multiple stakeholders, must logically be handled rather like money, by the owning citizens themselves, or by trusted professional data bankers or some other such trusted third-party brokers. Citizens will need something akin to a personal data transactions account, rather like a personal money transactions bank account. Consent will be akin to specific delegated Power of Attorney, allowing others to work with and manage the data in the account. Governance of this arrangement will formalize the delegated authority of the citizen and professional co-creators of the data, to manage the data on their behalf.
Foremost in formalizing the governance of personally owned data is the need for common ground that values the preservation of its meaning, couched within context, and its appropriate, timely and efficient communication–seamlessly, coherently, understandably and inclusively. This is the nature of the information governance that is required for oversight of the groupings of personal data that I have characterized as ‘omnuscular’, in Chapter Three. Where non-coherent data sources proliferate and multiply, there is risk of noise, bias, discontinuity and imbalance in the uses made of them, and how these interact. Such incoherence may be costly, harm or impede health care, obstruct capacity to innovate, cause frustration and erode and destroy trust.
A long-term task in Implementation Three will be one of learning how to enact personal information governance centred on changing and trusted values and principles. This will play out over a Kahneman twenty-year timescale, at least. It will need to be locally enacted, within a globally-evolved framework of methods and regulations. For this to be feasible, a common ground of information architecture, adequate to the task, will be essential. Chaotic diversity of intercommunicating database and knowledge representation architectures will lead to biased and noisy judgements.
In all this, we must be mindful that not universally, and not always, will patients wish to avail themselves of the transparency enshrined in a right of access to their care records. For some patients, a terminal diagnosis will feel best left unknown. There will also be understandable caution among clinicians–for example, in committing suspicion of child abuse to a likewise transparent clinical record. Clinical information governance must seek to accommodate such realities safely, for all concerned.
This set of imponderables and their implications for governance and leadership are not new but have become much amplified in the Information Age. Alongside governance, one further issue now stands out as requiring new ideas for the creation of the care information utility. In parenthesis of this chapter, I reflect on alliance.
Parenthesis–Alliance
Sun Tzu’s writing, from long ago, mapped the different characteristics of battle terrain and described the importance of developing strategy within context. It is remarkable how it has endured as a course text of leadership academies, to this day. The terrain of health informatics is in parts blocked at a crossroads, on intractable ground, and it needs to be opened up. Strategy in such contexts is well-captured in his words, here:
[...] On open ground,
Do not block.
On crossroad ground
Form alliances.
[…] On intractable ground,
Keep marching.103
There has been a blockage of open ground–we have seen this as a characteristic of challenged leaders on landscapes navigated by great innovators in history. We have needed to keep marching on intractable ground through the Information Age, for fifty years. And we are now at a crossroads, halfway to the Information Society. We need to be good at building alliances.
Building good alliances is a social skill and I have learned from and been good friends with some outstanding builders of alliances. Alliances do not always endure or work out, but they are essential for sustained progress in complex, multi-sector and multifactorial domains, like health informatics. Here is one story to end with.
In my early twenties, I saw how life experience as refugees in wartime motivated the individuals and teams that created Amnesty International. I saw this from a time of small evening gatherings of like-minded citizens, including lawyers, businesspeople and politicians, in pubs just off Fleet Street in London. That was Penrose stage one. I saw it grow through stages two and three, establishing a UK secretariat on which I served for several years with one of Amnesty’s co-founders, Eric Baker (1920–76), my then wife, Jenny’s, dad. It grew into an international community, with national affiliated movements and an overarching board, where Eric was a founding member and voice for its mission. He had worked alongside his co-founder, Peter Benenson (1921–2005) from Amnesty’s earliest days in the 1960s. The international scene was then led by Seán MacBride (1904–88), a prominent Irish politician (son of the English-born Irish republican revolutionary, suffragette and actress Maud Gonne) who briefly led the IRA, subsequently serving on the Council of Europe and at the United Nations. He was awarded the 1974 Nobel Peace Prize. A thought-provoking example of allegiance and alliance in pursuit of the resolution of intractable challenge!
All this sprang into life after Benenson’s article in the Observer, entitled ‘The Forgotten Prisoners’ (Prisoners of Conscience, Amnesty termed them).104 It caught a concern, established a common ground for campaign and connected groups of citizens with practical support for families and advocacy on behalf of individuals imprisoned. Leaders of industry, musicians, politicians and many others found common ground and common cause, and created vibrant concerted action that spread worldwide. It had and continues to have its noisy and complex ups and downs.
Witness the individual human focus, the alliance of community interest on a common ground of concern, the local and global impact, affiliation and governance, the organization to scale through four Penrose squared levels of endeavour. openEHR is happening and progressing to level four. openCare can happen, too. It can be made, and it can be done!
1 Adventures of Ideas (New York: Macmillan, 1933), p. 248.
2 Ibid., p. 247.
3 M. King, The End of Alchemy: Money, Banking and the Future of the Global Economy (New York: W. W. Norton and Company, 2016).
4 As I finalize this section in the weeks ahead of my self-imposed publisher deadline, the Times newspaper has an article by the economists, Mariana Mazzucato and Rosie Collington, presaging their new book, The Big Con: How the Consulting Industry Weakens Our Businesses, Infantilizes Our Governments and Warps Our Economies (London: Allen Lane, 2023). The article title is more explicit still–‘Trillion-dollar Con Trick: Advice that Makes Things Worse’ (The Times (10 February 2023), https://www.thetimes.co.uk/article/trillion-dollar-con-trick-advice-that-makes-things-worse-pgrs5jc5j). Confidence tricks take us down–be they by sleight of hand, deceit, hubris or pretence of knowledge. Intentionally or otherwise, they break faith and trust. We must not mix up our cons and contras, though. Con- is about togetherness. We need new confidence and conviction to conjoin and connect in ways that help us back up and help keep us there in matters of health care. The idea of care information utility, as developed in this book, is as a common ground of implementation of information utility, towards that (convivial!) human end.
5 Congress of the United States Office of Technology Assessment, Policy Implications of Medical Information Systems (Washington, DC: Congress of the United States Office of Technology Assessment, 1977), https://www.princeton.edu/~ota/disk3/1977/7708/7708.PDF
6 R. E. Susskind and D. Susskind, The Future of the Professions: How Technology Will Transform the Work of Human Experts (Oxford: Oxford University Press, 2015), p. 46.
7 G. Tett, Anthro-Vision: A New Way to See in Business and Life (New York: Simon and Schuster, 2021).
8 Computers tend to work or not to work. Their designs have limitations, exhibit behaviours and develop faults. Mine is five years old and suffering from ailing silicon joints, and slow performance on the increasingly demanding machine racecourse that Microsoft sets programs to run on. No doubt this reflects the greater complexity of the computer and increased attack from data highway robbers in the global environment of computers, today. If all else fails, I can buy a new machine and be assisted for my purposes by this more athletic and less accident-prone young device. I can revert to handwriting, but even paper and ink can run out and pens and fingers fail. I balance the costs and benefits and make a choice. Health care is not like this. The body can be measured and imaged to the limits of the capability and capacity of the Information Age, but if we look for dysfunction, we will surely find it somewhere, but so what? Back pain may be investigated with imaging devices and an MRI will find ageing joints. The significance of findings and the choice of remedial action are wide-ranging in context and efficacy. The reporting and interpretation of the pain will likewise reflect the human subject in pain–some more Stoic and able to cope than others. Treatment may involve analgesia, acupuncture, physiotherapy, surgery–it can give some help and cause some harm. Unlike with the machine, a new back is not (yet!) an option–we must cope and be helped to cope with the reality as best possible. Machine virtual realities may usefully complement and enhance human realities and they may conflict or prioritize differently. My back is not a machine that can be conjured back to life. But both machine and back have patterns of behaviour and trade-offs in how we chose and accommodate them. In how we mix the two and how we use them–individually and in combination.
9 C. Christensen, M. E. Raynor and R. McDonald, Disruptive Innovation (Boston, MA: Harvard Business Review, 2013).
10 On Globalton and Localton, see Chapter Seven.
11 On this Polish expression, see Preface.
12 L. S. Penrose, ‘The Elementary Statistics of Majority Voting’, Journal of the Royal Statistical Society, 109.1 (1946), 53–57.
13 Nearly twenty years ago, I attended a lavish party celebrating one of the first awards of major contracts under the ill-fated NHS Programme for IT. This was for a hospital-wide patient administration system. The successful company surged in value on the news. Its owners quickly sold out. The ‘bonnet’ of the system purchased was lifted by the hospital team. I was told that much of the engineering was ancient, key aspects of the product a poor fit, and the necessary reengineering to make them fit, costly and time-consuming. Tens of millions of pounds of direct and indirect cost and disruption ensued. The system has since been replaced.
14 M. Obama, The Light We Carry: Overcoming in Uncertain Times (London: Penguin Books, 2022).
15 The Nordic countries include the sovereign states of Denmark, Finland, Iceland, Norway and Sweden as well as the autonomous territories of the Faroe Islands and Greenland, and the autonomous region of Åland.
16 R. M. Axelrod, The Evolution of Cooperation (London: Penguin Books, 1990).
17 Benjmain Franklin at the signing of the Declaration of Independence, July 4, 1776.
18 M. J. Sandel, The Tyranny of Merit: What’s Become of the Common Good? (London: Penguin Books, 2020).
19 ‘Remembrances’, l. 67.
20 K. Popper, The Open Society and Its Enemies: The Spell of Plato (London: Routledge and Kegan Paul, 1957).
21 R. D. Putnam, The Upswing: How America Came Together a Century Ago and How We Can Do It Again (London: Simon and Schuster, 2020).
22 T. Piketty, A Brief History of Equality (Cambridge, MA: Harvard University Press, 2022).
23 L. A. Fennell, ‘Ostrom’s Law: Property Rights in the Commons’ (John M. Olin Program in Law and Economics Working Paper No. 584, 2011), p. 10, https://chicagounbound.uchicago.edu/cgi/viewcontent.cgi?article=1356&context=law_and_economics
24 Susskind and Susskind, Future of the Professions. One should note, however, that according to its founder, Jimmy Wales, typically only two percent of its users respond to a request to donate in support of the work it involves. This is not enough and Lionel Penrose’s ‘square root law’ might suggest that ten percent will be needed for it to be sustained and prosper.
25 C. R. Sunstein, Infotopia: How Many Minds Produce Knowledge (Oxford: Oxford University Press, 2006).
26 D. Kahneman, O. Sibony and C. R. Sunstein, Noise: A Flaw in Human Judgment (New York: Little, Brown Spark, 2021).
27 D. Kahneman, Thinking, Fast and Slow (New York: Macmillan, 2011).
28 Whitehead was more incremental in his thinking than this, as the quotation heading Part Three of this book indicates. I suspect few if any wicked problems will succumb to being driven rapidly to scale. Of course, the larger and more diverse the entity wherein we seek to engender change, the harder moving quickly to scale becomes. The greater success of smaller jurisdictions in successful implementation of health care information policy is significant. Anecdotally, an upper limit of around fifteen million in the target population seems to have proved a tipping point, from achievable to unachievable success. However, I have observed representatives of such smaller and successful countries bristle at the suggestion that they might be more successful because smaller!
29 I recalled noting in my talk for a UK/USA intergovernmental conference of 2004, on the role of informatics in improving the quality of health care, that failure of attempts to drive innovation successfully to scale had bedevilled health care information policy from the beginning. This was picked up on later, and wise heads from right across governments nodded, but it was not seen as anyone there’s problem.
30 M. Mazzucato, The Entrepreneurial State: Debunking Public vs. Private Myths in Innovation, rev. ed. (London: Anthem Press, 2014).
31 Piketty, Brief History, p. 2.
32 Ibid., p. 10.
33 Ibid., p. 12.
34 Ibid., p. 13.
35 Ibid.
36 Ibid.
37 Ibid., p. 15.
38 Ibid., p. viii.
39 Ibid., p. 244.
40 Mazzucato, Entrepreneurial State.
41 L. Carroll, ‘The Hunting of the Snark’, ll. 1–8.
42 E. Topol, Deep Medicine: How Artificial Intelligence Can Make Healthcare Human Again (London: Hachette, 2019).
43 Much of the advocacy of FHIR and openEHR as alternatives (it used to be GEHR and HL7–Version 3!) in argumentation about digital care record interoperability has invoked false dichotomy, in my view. They have addressed different requirements–one of communication of information between systems and the other of architecture and persistence of care record systems, themselves. In those respects, the one cannot subsume the other’s design, although they will, of course, interrelate. They can both be good and succeed, or be bad and fail. Their balance is not about information technology alone–it is a matter of the purposes they serve and their sustainability over time–in other words about implementation. Better by far, to implement, balance and broker them in the sense of dualism, and find common ground. I have not had the time or energy to engage in false dichotomy and others are better than me at debating the dualisms. I have had the privilege and preference to create and lead an environment where we implemented meaningful concepts for practical use and debate, rather than merely confabulating ideas about what might be possible but never quite materialized!
44 D. Goodhart, Head Hand Heart: The Struggle for Dignity and Status in the 21st Century (London: Penguin Books, 2020).
45 Topol, Deep Medicine.
46 This was when I was preparing the 1991 Royal Society of Medicine talk on this theme, that I was asked to give at the halfway point of my career. The notes prepared for this talk are available at https://www.openbookpublishers.com/books/10.11647/obp.0335#resources
47 On the hedgehog/fox classification, see Chapter Eight.
48 Quote attributed to Nelson Mandela (2001).
49 C. Naylor, ‘The Case for Public Service Reform’, BBC Radio 4 (6 March 2022), https://www.bbc.co.uk/programmes/m0014x7v
50 M. C. Escher, ‘Circle Limit III’, Wikimedia Commons (3 February 2015), https://en.wikipedia.org/wiki/Circle_Limit_III#/media/File:Escher_Circle_Limit_III.jpg. This woodcut was inspired by the work of the French mathematician Jules Henri Poincaré, bounding the whole of an infinite flat plain within a finite circle. Escher was inspired by the marvelous designs of nature and mathematics and an artistic approach to infinity.
51 See Chapter Eight.
52 Axelrod, Evolution of Cooperation.
53 A. Einstein, Ideas and Opinions (New York: Crown Publishers, 1954), p. 271.
54 Lao Tzu (sixth century BC), Tao Te Ching, trans. C. Q. Wu, Thus Spoke Laozi: A New Translation with Commentaries of Daodejing (Honolulu: University of Hawaii Press, 2016), p. 137.
55 M. C. Escher, ‘Tower of Babel’, Digital Commonwealth, https://www.digitalcommonwealth.org/search/commonwealth:3r076t25f
56 F. P. Brooks Jr., The Mythical Man-Month: Essays on Software Engineering (New Delhi: Pearson Education, 1995).
57 S. Simard, Finding the Mother Tree: Uncovering the Wisdom and Intelligence of the Forest (London: Penguin Books, 2021).
58 In my UCL/CHIME years, from 1995–2012, two anthropologists worked with us and nearby. Paul Bate specialized in organizational development of health services and Cecil Helman (1944–2009), working in our neighbouring, closely allied Primary Care Department. Paul made a much-valued contribution to our graduate health informatics programme, and Cecil, world-renowned for his book Culture, Health and Illness, 4th ed. (Oxford: Butterworth/Heinemann, 2000), which went to five editions, was an interesting and educative person to talk to at lunch times in the canteen. It was a richly creative environment in its time.
59 Axelrod, Evolution of Cooperation; R. Fisher and W. Ury, Getting to Yes: Negotiating Agreement without Giving In., 2nd ed. (New York: Penguin Books, 1991).
60 Sepsis Trust, https://sepsistrust.org/
61 Kahneman, Sibony and Sunstein, Noise: A Flaw.
62 Many very successful people I have known, whose contributions have bridged between information technology and health care, have occupied niche positions situated at a safe distance from the pressures faced in mainstream environments combining academic medicine and health care practice: in academic computer science, epidemiology and public health, medical physics, professional organizations and biomedical technology research centres. Others took a special interest in informatics and combined this with clinical professional and academic roles. In America, stellar early careers in the field have bridged the heights of academic medicine and informatics, benefiting from wealthy sponsoring institutions and substantial government pump-priming funds. Some of their colleagues established companies and became very rich.
63 There were, for example, many tens of separately configured and managed email servers operating across the UCL community, each run by a small team determinedly defending its own base. These local teams also provided locally configured scientific and administrative support services for their local academic colleagues, who, in turn, feared loss of local budget and services that they depended on, following merger into a central university service. Each local community deployed arguments of exceptionalism and deployed the power of its strong and exceptional leaders to defend their interests. The ensuing dialogue played out the universal narrative of global versus local interests. This was a fragmented, costly and vulnerable community and scene, and its tensions absorbed too much resource and effort. It knew that it had to change, but individual components feared disadvantage and there was resistance to change. The central UCL IT department was a battle-hardened environment and reluctant to countenance federated arrangements. It had enough on its hands in holding together all the other central academic services departments and their separate relationships with the arts and humanities, law, science, medicine, built environment, and engineering academic faculties. The same issues of integration and teamwork arose with all of these, in context of libraries, estates, finance, human resources and so on. One of my delegated roles, over time, was to gain the trust of both ‘globalizers’ and ‘localizers’ across the whole of UCL Biomedicine, and, with strong backing from the Deans and Directors involved, work constructively with both, to temper inevitable power plays and encourage cooperation. That meant years of regular engagement, helping find and implement a good way forward for the many highly-motivated people employed, focused on getting them involved in creating a better and more cost-effective future working environment, for UCL and for themselves.
64 N. McIntyre, How British Women Became Doctors: The Story of the Royal Free Hospital and Its Medical School (London: Wenrowave Press, 2014).
65 It had been part of the expectation in our recruitment to UCL that I would engage in supporting change in all these dimensions, and this took considerable time and energy, alongside the work of building and supporting the team for the new department’s academic mission. To those ends, I was appointed, over time, to central UCL IT and finance committees and the biomedicine executive, as well as to the board of academic heads of department of UCL, working for successive Provosts and Deans. Seen as a flag carrier for such a contentious field as that linking IT and health care, this placed me close to the front lines of many institutional dialogues and rivalries, both within the University and in its relationship with local and national NHS organizations and activities. I saw these roles as somewhat akin to those of Francesca Wilson, working as she described in In the Margins of Chaos: Recollections of Relief Work in and between Three Wars (New York: Macmillan, 1945). In such situations, how a goal is tackled is as impactful as how it is defined. It was a checkered history—some of it successful and some less so. Among my consequential relationships of those times were those with successive UCL Vice-Provosts, Deans and Vice-Deans of the Medical School—John Pattison, Roland Levinsky (1943–2007), Dave Delpy, David Price, David Patterson, Robert Souhami, Michael Spyer, Leon Fine, Ed Byrne and Ian Jacobs, and with Cengiz Tarhan as head of UCL Business.
66 Leon subsequently became Dean of the Medical School and brought me onto his executive team, where I remained with all subsequent Deans. When he returned to the States some years later, he contacted me as I neared retirement, asking if I would consider joining him at Cedars-Sinai, Los Angeles, I think it was, to help sort out their informatics services, as I had been doing for UCL Biomedicine, for him and the other UCL Clinical Deans. It would not have worked for us, but it was nice to be asked.
67 A. Gawande, Better: A Surgeon’s Notes on Performance (New York: Metropolitan Books, 2007).
68 Goodhart, Head Hand Heart; Sandel, Tyranny of Merit.
69 M. Sandel, What Money Can’t Buy: The Moral Limits of Markets (New York: Farrar, Straus and Giroux).
70 Topol, Deep Medicine.
71 Tett, Anthro-Vision.
72 Putnam, Upswing.
73 Susskind and Susskind, Future of the Professions, p. 43.
74 M. Roberts, ‘Machine Churning’, New Scientist, 250.3335 (2021), 23, https://doi.org/10.1016/S0262-4079(21)00873-3
75 M. Roberts et al., ‘Common Pitfalls and Recommendations for Using Machine Learning to Detect and Prognosticate for COVID-19 Using Chest Radiographs and CT Scans’, Nature Machine Intelligence, 3.3 (2021), 199–217.
76 Roberts, ‘Machine Churning’, p. 23.
78 Topol, Deep Medicine, p. 26.
79 ABBA, ‘Money, Money, Money’, Arrival (1976).
80 Lao Tzu, Tao Te Ching, trans. Wu, p. 40.
81 Quote attributed to Charles Darwin.
82 ‘Adam Galinsky: What Drives Us to Speak Up?’, TED Radio Hour (7 April 2017), https://www.npr.org/2017/04/07/522857511/adam-galinksy-what-drives-us-to-speak-up
83 D. de Rougemont, Penser avec les Mains (Paris: A. Michel, 1936).
84 Goodhart, Head Hand Heart.
85 J. Minford, trans., Sun Tzu: The Art of War (London, Penguin Group, 2002).
86 De Rougement, Penser avec les Mains, pp. 146–47. Translation using Google Translate.
87 Sun Tzu, Art of War, trans. Minford, p. 1.
88 Ibid., pp. 7–8.
89 Ibid., p. 12.
90 Ibid., p. 20.
91 Ibid., p. 21.
92 Ibid., p. 36.
93 Ibid., p. 37.
94 Ibid., p. 43.
95 Ibid.
96 Ibid., p. 17.
97 Ibid., p. 91.
99 W. S. Gilbert, Ruddigore, Act 2.
100 W. S. Gilbert, The Mikado, Act 2
101 W. S. Gilbert, The Gondoliers, Act 2.
102 Kahneman, Sibony and Sunstein, Noise: A Flaw.
103 Sun Tzu, Art of War, trans. Minford, p. 75.
104 P. Benenson, ‘The Forgotten Prisoners’, Observer (28 May 1961).